What is Pancreatitis?
Pancreatitis is inflammation of the pancreas. It happens when digestive juices or enzymes attack the pancreas gland itself.
Pancreas lies behind your stomach. It produces enzymes like amylase, lipase, protease, and trypsinogen for absorption. Through the pancreatic duct, it secretes digestive fluids into the small intestine. The pancreas also releases the hormones glucagon and insulin into circulation.
There are two types of Pancreatitis: acute Pancreatitis and chronic Pancreatitis.
Don’t miss out on any health updates
What is chronic Pancreatitis?
The chronic pancreatic disorder is the progressive inflammation of the pancreas. It does not heal or improve but worsens over time, leading to permanent damage. In severe cases, it may cause the pancreas to stop making digestive enzymes and insulin.
Learn more about chronic Pancreatitis down below:
What is acute Pancreatitis?
The acute pancreatic disorder is a sudden inflammation of the pancreas and usually goes away in a few days with treatment.
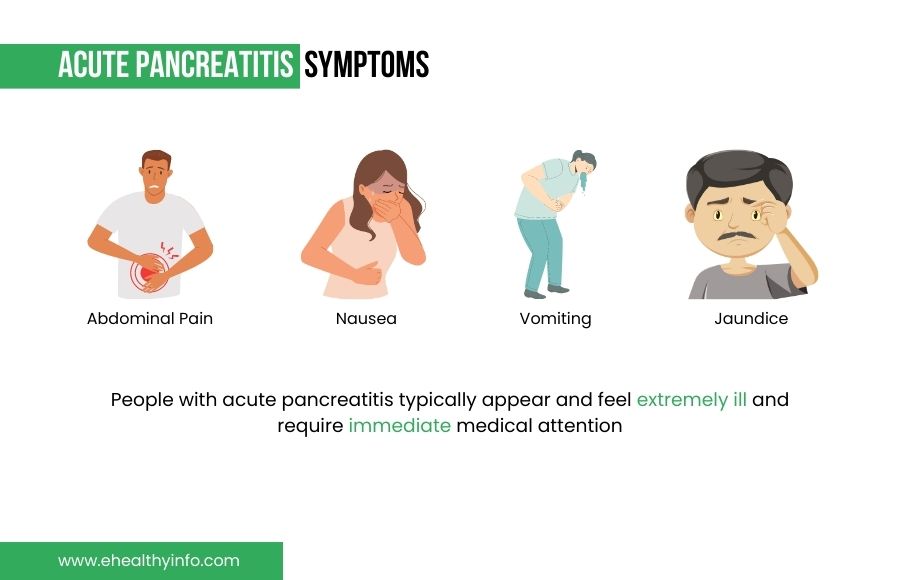
What are the Symptoms of Acute Pancreatitis?
The common symptoms of acute Pancreatitis are severe pain in the upper abdomen, nausea, and vomiting. The abdominal pain can be constant and radiate to your back. In gallstone pancreatitis, you can have yellowish discoloration of the skin and eyes (jaundice). People with acute pancreatitis typically appear and feel extremely ill and require immediate medical attention.
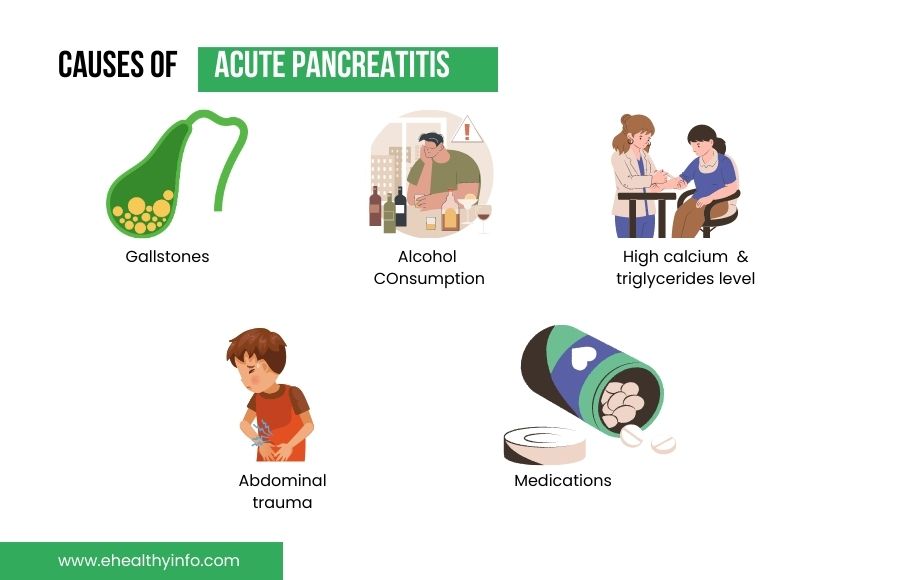
What causes Acute Pancreatitis?
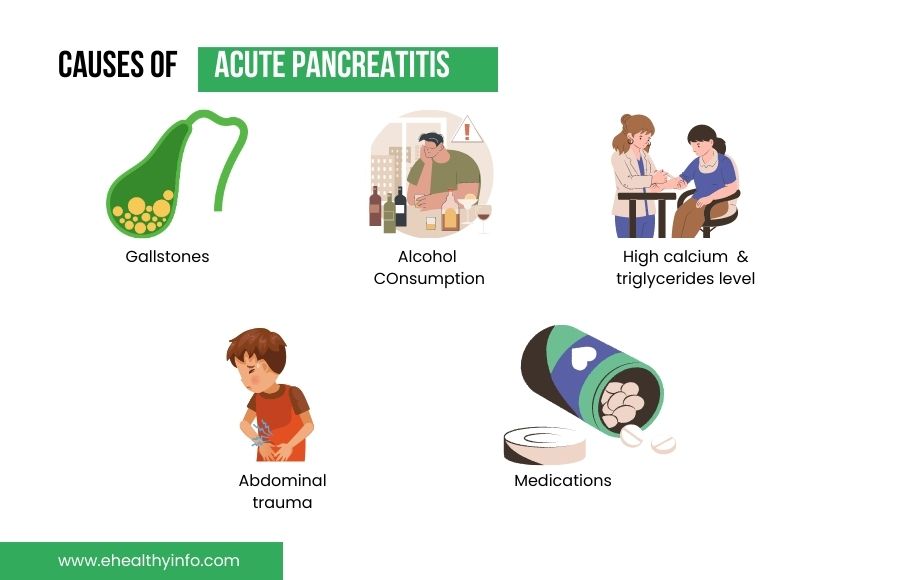
- Gallstones: The most common cause of acute Pancreatitis is gallstones. As the stones pass through and become lodged in a bile or pancreatic duct, the gallstones can result in pancreas inflammation.
- Alcohol Consumption: Heavy alcohol use is related to pancreas inflammation
- High blood levels of calcium (usually due to other medical problems)
- High blood levels of triglycerides (a particular type of fat in the blood)
- Abdominal trauma
- Inherited diseases affecting the pancreas, including cystic fibrosis
- Scorpion stings
- Viral infections (e.g., Coxsackievirus B, Mumps)
- Major surgery
- Medications like steroids, Azathioprine, Sulfonamides, Diuretics (loop and thiazide), estrogen, and drugs used for epilepsy (Sodium Valproate).
- Idiopathic -In many cases, doctors can’t find the cause of pancreas inflammation. This is called idiopathic Pancreatitis
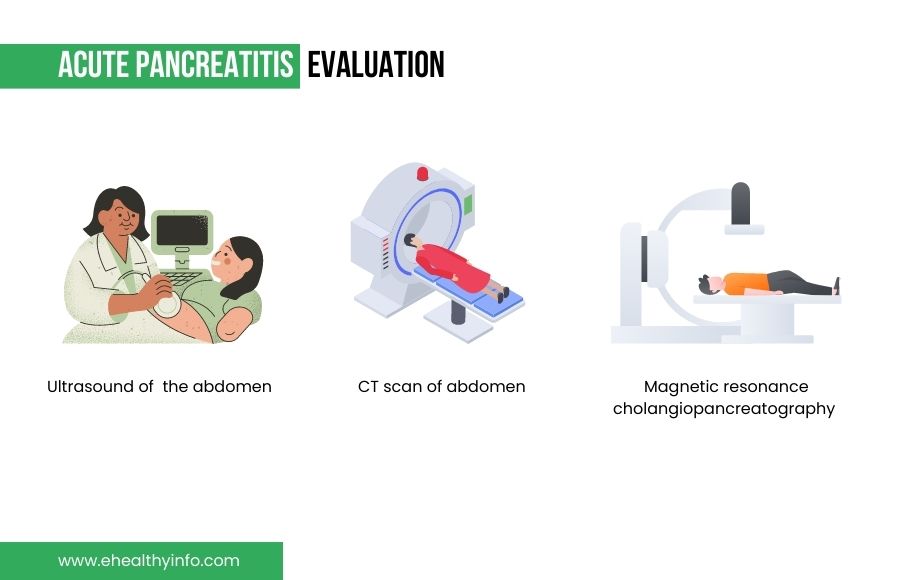
How will your doctor evaluate an acute attack of Pancreatitis?
Your doctor will do a clinical examination, order laboratory tests, and radiological imaging (USG or CT scan) of the abdomen. Your doctor will ask about your symptoms and the duration of the symptoms. Your doctor will also inquire about any medications you have been taking recently. A personal or family medical history of pancreas inflammation or gallstones is important for your healthcare provider.
Your doctor can diagnose pancreas inflammation if you have abdominal pain, a high amount of lipase and amylase in the blood (enzymes made by the pancreas), and imaging findings suggestive of pancreatic inflammation.
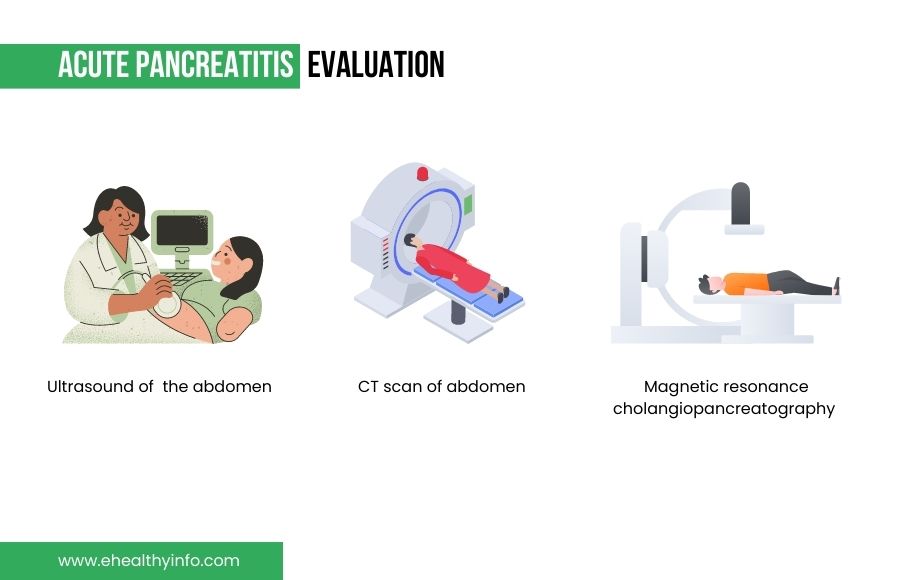
Ultrasound: Ultrasound is painless sound waves to create a picture. Ultrasound can find gallstones.
CT scan of the abdomen: It gives a clear picture of your pancreas, gallbladder, and bile ducts. CT scans can show pancreas inflammation or pancreatic cancer.
Magnetic resonance cholangiopancreatography (MRCP): MRCP uses a magnetic resonance imaging (MRI) machine to provide images of your organs and soft tissues without using X-rays. Your pancreas, gallbladder, and bile ducts may be examined using MRCP by your doctor or a specialist to look for causes of pancreas inflammation.
How is Acute Pancreatitis treated?
The goal of treatment is to rest the pancreas and let it settle down. You will need to be hospitalized and stay there for a few days.
- Bowel rest
- Intravenous fluids for hydration and to balance electrolytes
- Intravenous pain medications
- Endoscopic Cholangiopancreatography (ERCP): To treat a bile or pancreatic duct obstruction or narrowing, ERCP combines upper gastrointestinal endoscopy and x-rays. Gallstones that obstruct the bile or pancreatic ducts can be removed with ERCP by your gastroenterologist.
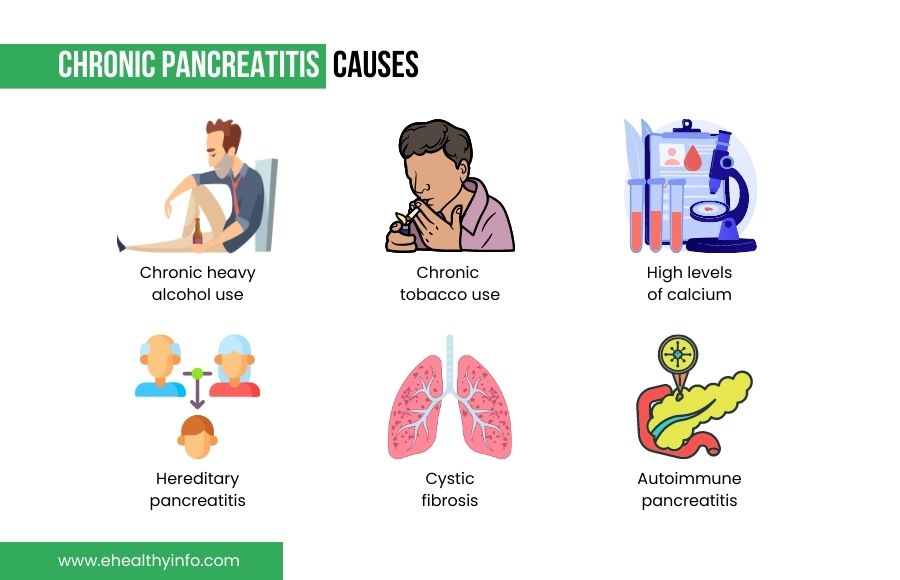
What are the causes of Chronic Pancreatitis?
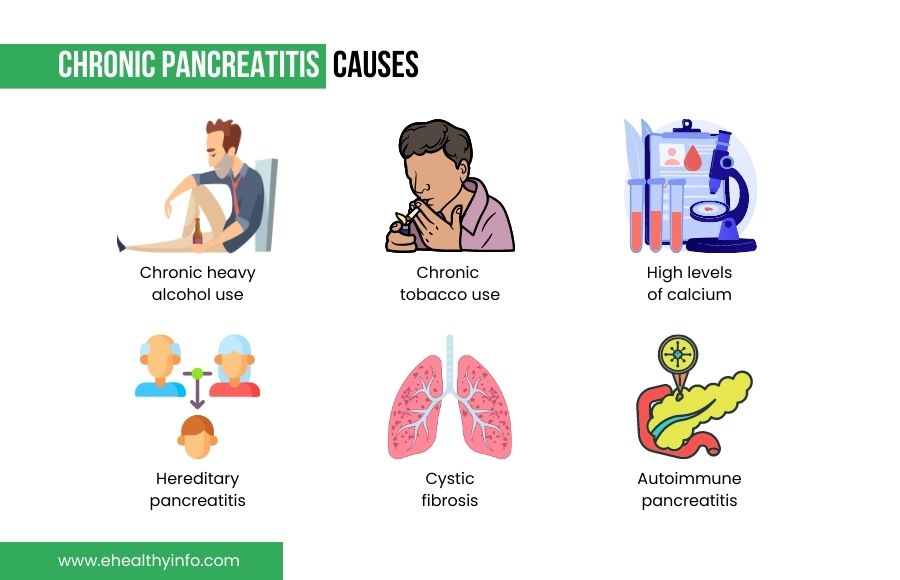
- Chronic heavy alcohol use
- Chronic tobacco use
- High levels of calcium
- Hereditary Pancreatitis
- Autoimmune Pancreatitis
- Cystic fibrosis
How will your doctor diagnose Chronic Pancreatitis?
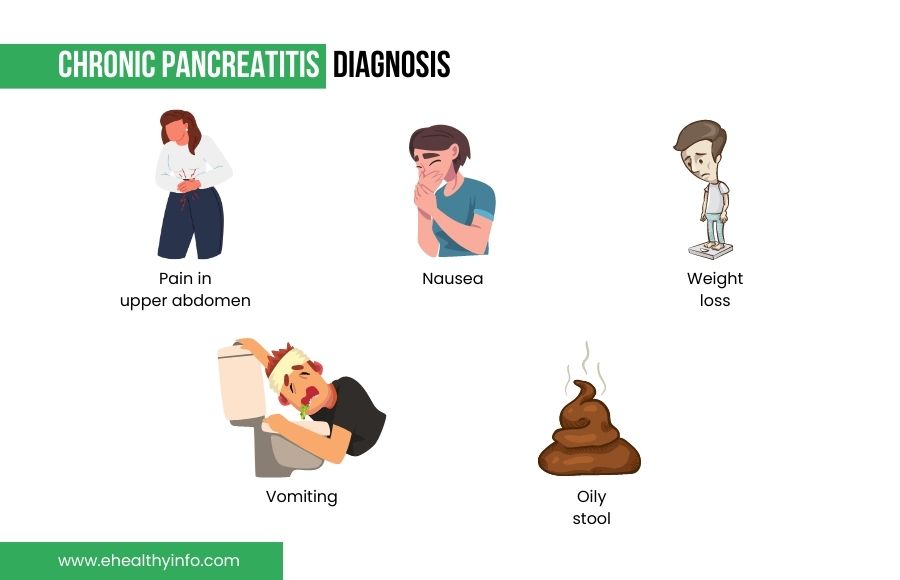
Most people with chronic Pancreatitis have no symptoms. Patients can have chronic pain in the upper abdomen, nausea, vomiting, weight loss, and oily stools. Your doctor will do clinical examinations, lab tests, and imaging to diagnose chronic Pancreatitis. Imaging studies like CT scans and magnetic resonance cholangiopancreatography (MRCP) might show calcifications, ductal dilations, and small and fibrosed pancreas.
How is Chronic Pancreatitis treated?
Treatment for chronic Pancreatitis involves the management of chronic pain and manage complications.
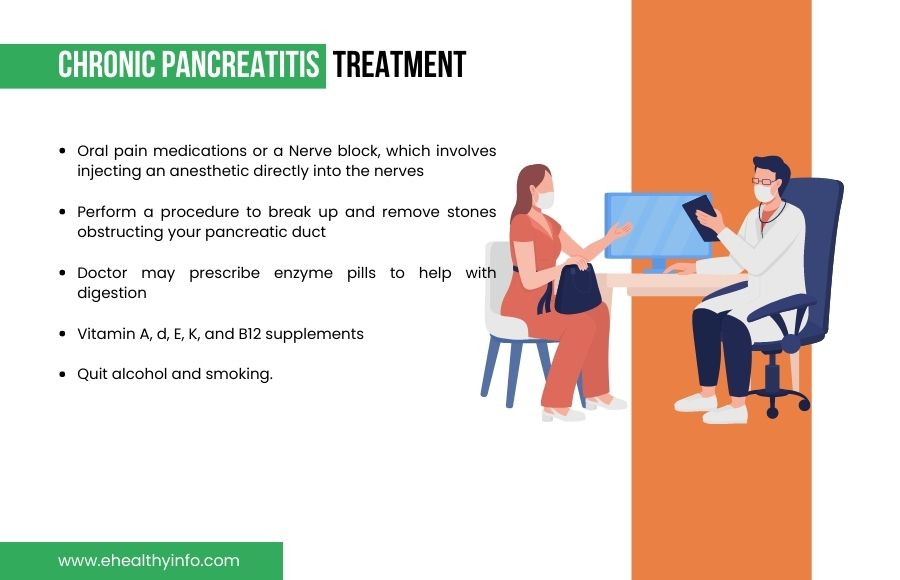
- Non-steroidal anti-inflammatory drugs (NSAIDs) are recommended for pain management. Your doctor might advise a nerve block, which involves injecting an anesthetic directly into the nerves that transport pain signals from your pancreas via your skin.
- If you have stones in this area, your doctor may perform a procedure to break up and remove stones obstructing your pancreatic duct.
- Diabetes may result from chronic pancreas inflammation. If you get diabetes, your doctor and medical team will collaborate with you to develop a diet plan, a medication schedule, a blood glucose monitoring regimen, and regular exams.
- Your doctor may prescribe enzyme pills to help with digestion. You may need to take frequent small meals to aid in digestion.
- You might be deficient in multivitamins due to malabsorption- You might need Vitamin A, d, E, K, and B12 supplements.
- Quit alcohol and smoking.
What are the complications of Pancreas inflammation?
Acute Pancreatitis usually gets better on its own. A few cases result in fluid collections around the pancreas called pancreatic pseudocyst that requires drainage. Most people recover without any problems.
Chronic pancreatitis may improve independently but take longer due to repeated attacks.
Patients with chronic pancreas inflammation are at a greater risk of long-term problems.
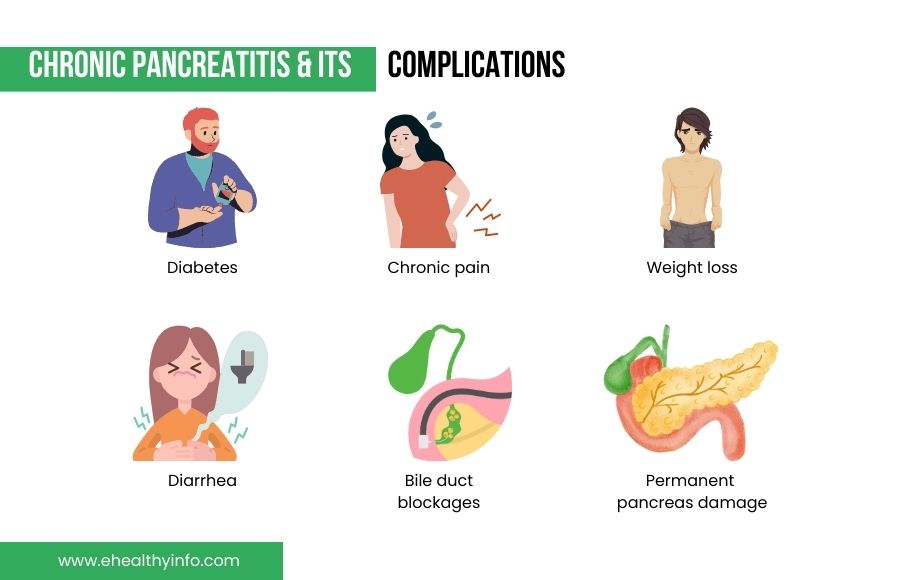
- Diabetes
- Chronic pain
- Diarrhea
- Weight loss
- Low vitamin levels from malabsorption
- A collection of fluid (pseudocyst) around the pancreas
- Bile duct blockages
- Permanent pancreas damage
Malabsorption in Chronic Pancreatitis
In Pancreas inflammation, the inflammation can disrupt the normal function of the pancreas, leading to malabsorption of nutrients from the food we eat. Malabsorption can occur because the digestive enzymes produced by the pancreas are not being released properly, leading to poor absorption of nutrients such as fats, proteins, and carbohydrates. This can result in weight loss, nutrient deficiencies, and other complications.
If you have malabsorption, your doctor may prescribe enzyme supplements or the vitamins NA, D, E, and K. You could require vitamin B-12 because of malabsorption.
Nutrition recommendations for Chronic Pancreatitis?
- Follow a low-fat diet that, depending on tolerability, is frequently limited to 50 grams of fat.
- If you have diabetes, talk to a dietician and manage your serving sizes of low-fat carbohydrates to help control blood sugars (low-fat/nonfat dairy, fruits, vegetables, whole grains, beans, lentils, etc.)
- Take pancreatic enzymes as directed by your doctor
- Take the pancreatic enzymes before each meal and snack. They will not work if taken at the end of the meal.
Tips for a low-fat diet
- Eat 4-6 small meals throughout the day.
- Distribute the fat you consume throughout the day.
- Sparingly use butter, margarine, and cooking oils.
- Foods can be steamed, grilled, baked, or roasted. Do not fry or stir fry foods.
- Include fruits, vegetables, whole grains, and low-fat/nonfat dairy daily
- Add protein to each meal (lean beef, chicken without skin, fish, low-fat/nonfat dairy, egg whites, beans, soy)
- Avoid all alcohol products.
How to prevent yourself from developing Pancreas inflammation?

- Avoid Drinking Alcohol.
- Do not smoke cigarettes.
- Eat a small frequent healthy diet.
- Eat food with a good amount of protein and carbohydrates and less fat
- Drink plenty of fluids and limit caffeine
- Exercise at least 30 min/per day, five days/week
Questions for your doctor
- How can I manage the pain associated with pancreas inflammation?
- What can I eat or drink while I have Pancreatitis?
- How long will it take for me to recover from pancreas inflammation?
- Are there any long-term effects or complications I should be aware of?
- Is there a way to prevent Pancreatitis from recurring?
- Can pancreas inflammation be a sign of a more serious underlying condition?