Acute Respiratory Distress Syndrome -Symptoms, Diagnosis, Treatment and Recovery

Highlights of Acute Respiratory Distress Syndrome (ARDS)
- Acute Respiratory Distress Syndrome is a severe and life-threatening lung condition that causes low blood oxygen levels, leading to shortness of breath and bluish discoloration of the skin and lips.
- Sepsis is the leading cause of ARDS.
- Acute respiratory distress syndrome treatment focuses on supportive management and ventilator support to enhance oxygen levels and maintain lung function.
- A tracheostomy often becomes necessary as part of acute respiratory distress syndrome treatment for those who experience prolonged ARDS.
- While some individuals may recover fully within weeks to months, others may experience long-term lung damage and require ongoing medical care, and in severe cases, it can lead to death.
What is Acute Respiratory Distress Syndrome (ARDS)?
Acute respiratory distress syndrome (ARDS) is a severe and life-threatening lung condition that causes low blood oxygen levels and “stiff” lungs. It occurs when the tiny air sacs in your lungs, called alveoli, get damaged. These alveoli are essential because they allow oxygen and carbon dioxide to be exchanged. When they’re damaged, fluid leaks in, making it hard for your lungs to do their job. This damage also causes inflammation and breaks down a substance called surfactant, which keeps the alveoli open. Lung infections, inhalation of smoke, or other illnesses and injuries that cause lung inflammation can cause this damage.[1]
Causes and Risk Factors of ARDS
Risk factors for ARDS include:
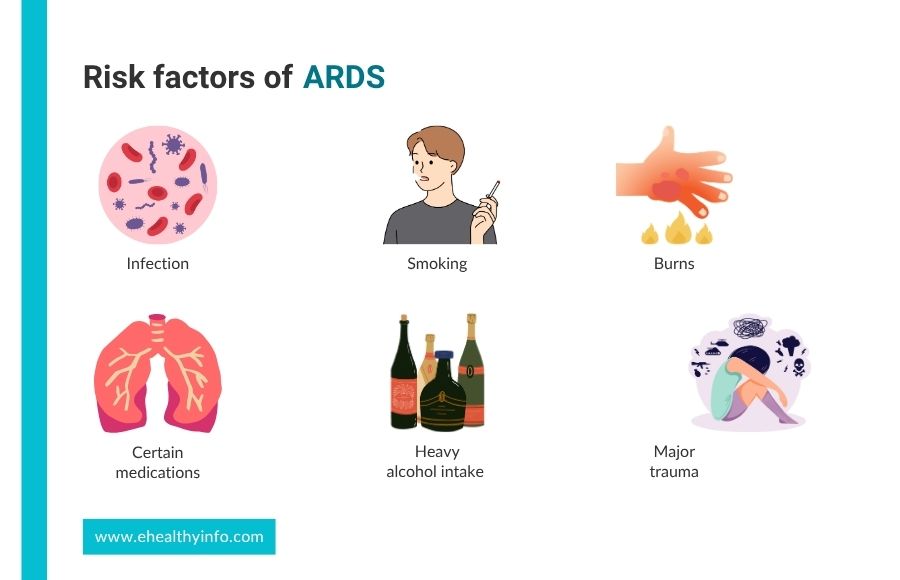
1. Infections
Sepsis, which occurs when an infection spreads throughout the bloodstream, is the leading cause of acute respiratory distress syndrome. [2] Other common infections that can lead to ARDS include pneumonia and viral infections like the flu, respiratory syncytial virus, and COVID-19. [1]
2. Heavy Alcohol Use
If you drink too much alcohol, you’re more likely to develop ARDS. It harms your lungs by reducing an important antioxidant called glutathione, weakening lung walls and affecting your body’s ability to fight infections. [3]
3. Smoking
Smoking damages your lungs by irritating and inflaming the lung tissues, making them less effective at exchanging oxygen and carbon dioxide. Both active smoking and being exposed to smoke from others raise this risk. [4]
4. Medical Conditions/Procedures
Surgeries involving the heart or lungs and pancreatitis can be complicated with ARDS. [5]
5. Medications
Acute respiratory distress syndrome can be triggered by a variety of medications, particularly those that cause direct lung injury or provoke severe inflammatory responses. The common drugs known are chemotherapeutic agents like bleomycin and cyclophosphamide and antibiotics like nitrofurantoin and amphotericin B. [6]
6. Major Trauma or Burns
Big accidents or severe burns can harm your lungs directly or damage other parts of your body, leading to serious swelling and inflammation in your lungs. [1]
Symptoms of ARDS
The symptoms of acute respiratory distress syndrome typically develop quickly, within hours to a few days following the injury or illness. [7] Here are some of the symptoms to watch out for:

1. Shortness of Breath
The first sign of ARDS is usually difficulty breathing, often reaching distressing levels, and feeling as though they are suffocating. The effort required to breathe significantly leads to rapid, shallow breaths as the body attempts to intake more oxygen. [1]
2. Cough
Patients with ARDS often have a dry cough that produces little to no mucus. This cough can be persistent and aggravating, causing discomfort. [1]
3. Chest Pain
Many people with ARDS report chest pain, particularly when taking deep breaths or coughing. This pain is often due to the inflammation and fluid buildup in the lungs, making breathing movements painful. [1]
4. Fever
If ARDS is caused by an underlying infection, such as pneumonia or sepsis, patients may experience fever. The body’s immune response to infection often includes elevated temperature. [1]
5. Low Blood Pressure
Low blood pressure can occur, particularly if ARDS is caused by conditions like sepsis or severe trauma. Hypotension further complicates the body’s ability to deliver oxygen to tissues and can lead to organ dysfunction. [8]
Complications of ARDS
Acute respiratory distress syndrome can lead to numerous complications, affecting both short-term and long-term health. Major complications are:

- Pneumothorax: The use of mechanical ventilation, especially with high pressures, can cause air leaks in the lungs, filling air into the pleural cavity, a layer surrounding the lungs. [9]
- Ventilator-Associated Pneumonia (VAP): Patients with ARDS often require mechanical ventilation, increasing the risk of developing pneumonia due to prolonged intubation. [10]
- Sepsis: Acute respiratory distress syndrome can be both a cause and a consequence of sepsis, a life-threatening infection that can lead to widespread inflammation and organ failure. [10]
- Arrhythmias: Electrolyte imbalances and hypoxemia associated with ARDS can lead to abnormal heart rhythms. [11]
- Multi-organ failure: When organs don’t receive enough oxygen, they may not function properly or stop working. This can result in several organs failing simultaneously, posing a life-threatening situation. [2]
- Pulmonary Fibrosis: Prolonged ARDS can lead to the scarring and thickening of lung tissue, resulting in chronic lung disease and persistent respiratory difficulties. [1]
- Complications of hospital treatment: These can include blood clots from prolonged bed rest, muscle weakness, infections, stress ulcers, and mood disorders like depression. Long-term use of sedative medicines can also lead to problems with thinking and memory. [11,12]
Diagnosis of ARDS
The diagnosis of ARDS involves confirming the presence of ARDS and ruling out other potential causes of respiratory distress. Here are the key steps in diagnosing the condition:

1. Laboratory Tests
- Arterial Blood Gas (ABG) Analysis: ABG analysis measures oxygen and carbon dioxide levels in the blood. Patients with acute respiratory distress syndrome usually have severely low levels of oxygen despite receiving supplemental oxygen. [13]
- Blood Tests: Various blood tests can help identify underlying causes or associated conditions, such as infections, sepsis, or inflammation. Tests may include a complete blood count, blood cultures, and markers of infection or inflammation like C-reactive protein.
2. Imaging Studies
- Chest X-ray: A chest X-ray is the first imaging test used. It can show bilateral white lung areas, indicative of fluid accumulation, a hallmark of ARDS. These opacities are not due to heart failure or fluid overload. [14]
- Computed tomography (CT) scan: A CT scan of the chest can provide more detailed images of the lungs, helping to identify the extent and pattern of lung involvement and rule out other conditions such as pulmonary edema or pneumonia. [15]
- Echocardiogram: An echocardiogram may be performed to evaluate heart function and exclude cardiac causes of pulmonary edema, such as left heart failure or valvular heart disease. [11]
Treatment of ARDS
Acute respiratory distress syndrome is treated in an intensive care unit (ICU), with a focus on supporting the patient and addressing the condition’s underlying cause.

1. Ventilator Support
All patients with ARDS will require extra oxygen support, but sometimes, oxygen alone isn’t enough and can even harm the lungs. That’s when ventilator support becomes necessary, as it helps open up closed airspaces and makes breathing easier. It’s connected to the patient through a face mask or a tube inserted into the windpipe. [8]
2. Prone Positioning
If oxygen and ventilator treatments are high and blood oxygen remains low, patients might be turned onto their stomachs or facedown to increase oxygen levels in the blood. This is called prone positioning and can temporarily boost oxygen levels. [8]
3. Medications
- Sedatives and muscle relaxants: Sedatives help keep patients calm and help them breathe better during adjustment. Muscle relaxants are given to prevent coughing or gagging while on a ventilator or to reduce the amount of oxygen the body requires. However, they have significant side effects and need continuous monitoring. [16]
- Diuretics: Your doctor may prescribe diuretics to ARDS patients to increase urine production. This helps remove excess fluid from the body and prevents fluid buildup in the lungs. [17]
- Antibiotics: Suitable antibiotics are given to prevent and treat infections that might have led to ARDS. [16]
- Blood thinners: Blood thinners are given to prevent clot formation. Heparin is commonly used for adults with ARDS. [18]
4. Extracorporeal membrane oxygenation (ECMO)
ECMO is an advanced treatment where blood is taken out of your body, passed through a special membrane that adds oxygen, removes carbon dioxide, and then returns to your body. While this therapy can be effective, it’s not suitable for every ARDS patient and carries high risks. [8]
5. Physical Therapy
Physical therapy helps keep your muscles strong and prevents sores from developing. It can also shorten the time spent on a ventilator and help in post-hospital recovery. [8]
6. Pulmonary Rehabilitation
Pulmonary rehabilitation can increase your lung capacity, making it easier for you to breathe and improve your overall lung function. [19]
ARDS and Need for Tracheostomy
A tracheostomy often becomes necessary as part of their treatment for patients who experience prolonged ARDS. This procedure involves creating an opening in the neck to insert a tube directly into the windpipe, providing a stable airway and facilitating long-term mechanical ventilation. Tracheostomies are considered when conventional breathing support through an endotracheal tube is no longer sustainable or when prolonged ventilator support is anticipated. [20]
Tracheostomy allows for better patient comfort, reduced risk of complications from prolonged intubation, and easier management of respiratory secretions. However, the decision to perform a tracheostomy in ARDS cases is complex, considering factors such as the patient’s overall condition, prognosis, and the potential for recovery. [20]
Questions To Ask Your Doctor
- How long might my loved one need ventilator support for ARDS?
- What are the chances of complete recovery from ARDS?
- Can this happen again in the future?
- Will they require oxygen therapy after recovering from ARDS?
- How long will it take for someone to reach maximum recovery?
References
- Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Primers 2019;5(1):18.
- Xu Z, Huang Y, Mao P, Zhang J, Li Y. Sepsis and ARDS: The Dark Side of Histones. Mediators Inflamm 2015;2015:1–9.
- Lassen MCH, Skaarup KG, Sengeløv M, Iversen K, Ulrik CS, Jensen JUS, et al. Alcohol Consumption and the Risk of Acute Respiratory Distress Syndrome in COVID-19. Annals of the American Thoracic Society. 2021 Jun;18(6):1074–6.
- Zhang L, Xu J, Li Y, Meng F, Wang W. Smoking on the risk of acute respiratory distress syndrome: a systematic review and meta-analysis. Critical care. 2024 Apr 14;28(1).
- Zhou MT. Acute lung injury and ARDS in acute pancreatitis: Mechanisms and potential intervention. World J Gastroenterol 2010;16(17):2094.
- Özbek AE, Divrikoğlu YS, Yılmaz S, Aytaş NÜ, Çelik E. Nonsteroidal anti-inflammatory drug-induced acute respiratory distress syndrome. Am J Emerg Med 2018;36(10):1929.e1-1929.e2.
- Saguil A, Fargo M V. Acute Respiratory Distress Syndrome: Diagnosis and Management. Am Fam Physician 2020;101(12):730–8.
- Griffiths MJD, McAuley DF, Perkins GD, Barrett N, Blackwood B, Boyle A, et al. Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir Res 2019;6(1):e000420.
- Teo YX, Geetha HS, Mishra AK, Lal A. Pneumomediastinum and pneumothorax in acute respiratory distress syndrome (ARDS) patients: a narrative review. Mediastinum 2024;8:3–3.
- Luyt CE, Bouadma L, Morris AC, Dhanani JA, Kollef M, Lipman J, et al. Pulmonary infections complicating ARDS. Intensive Care Med 2020;46(12):2168–83.
- Niehues P, Wegner FK, Wolfes J, Willy K, Ellermann C, Vollenberg R, et al. Incidence and predictors of cardiac arrhythmias in patients with COVID-19 induced ARDS. J Cardiol 2022;80(4):298–302.
- Frank P, Batty GD, Pentti J, Jokela M, Poole L, Ervasti J, et al. Association Between Depression and Physical Conditions Requiring Hospitalization. JAMA Psychiatry 2023;80(7):690.
- Balzanelli MG, Distratis P, Lazzaro R, Pham VH, Del Prete R, Dipalma G, et al. The importance of arterial blood gas analysis as a systemic diagnosis approach in assessing and preventing chronic diseases, from emergency medicine to the daily practice. Eur Rev Med Pharmacol Sci 2023;27(23):11653–63.
- Papazian L, Calfee CS, Chiumello D, Luyt CE, Meyer NJ, Sekiguchi H, et al. Diagnostic workup for ARDS patients. Intensive Care Med 2016;42(5):674–85.
- Pesenti A, Musch G, Lichtenstein D, Mojoli F, Amato MBP, Cinnella G, et al. Imaging in acute respiratory distress syndrome. Intensive Care Med 2016;42(5):686–98.
- Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care 2019;9(1):69.
- Vignon P, Evrard B, Asfar P, Busana M, Calfee CS, Coppola S, et al. Fluid administration and monitoring in ARDS: which management? Intensive Care Med 2020;46(12):2252–64.
- Stammers AH, Tesdahl EA, Barletti S, Mongero L, Patel K, Mosca M, et al. Anticoagulant Use During Extracorporeal Membrane Oxygenation Using Heparin and Direct Thrombin Inhibitors in COVID-19 and ARDS Patients. J Extra Corpor Technol 2022;54(3):223–34.
- American Lung Association. ARDS Treatment and Recovery | American Lung Association [Internet]. Lung.org. 2019. Available from: https://www.lung.org/lung-health-diseases/lung-disease-lookup/ards/ards-treatment-and-recovery
- Battaglini D, Premraj L, White N, Sutt AL, Robba C, Cho SM, et al. Tracheostomy outcomes in critically ill patients with COVID-19: a systematic review, meta-analysis, and meta-regression. Br J Anaesth 2022;129(5):679–92.
Return to Home
