Addison’s Disease – Key Symptoms, and Proven Treatment Strategies

Key Highlights Of Addison’s Disease
- Addison’s disease is a rare condition where the adrenal glands do not produce enough cortisol and aldosterone. It is also known as adrenal insufficiency.
- Symptoms of adrenal insufficiency include extreme fatigue, weight loss, skin darkening, low blood pressure, salt cravings, low blood sugar, nausea, and vomiting.
- Addisonian Crisis is a life-threatening emergency triggered by stress, which causes very low blood pressure, severe pain, vomiting, and confusion. It requires an immediate medical attention.
- Treatment involves lifelong hormone replacement therapy with medications like hydrocortisone and fludrocortisone to replace cortisol and aldosterone.
- To prevent an Addisonian crisis, wear a medical alert bracelet, carry an emergency hydrocortisone injection kit, and increase medication during stress or illness.
What is Addison’s Disease?
Addison’s disease, also called primary adrenal insufficiency, occurs when the adrenal glands that lie on top of each kidney produce insufficient amounts of hormones. The gland is responsible for producing three hormones, namely, cortisol, aldosterone, and androgen. In adrenal insufficiency, the gland produces no or decreased amounts of cortisol and aldosterone, which are critical for maintaining balance in the body. Since cortisol regulates metabolism and the body’s response to stress, a deficiency can lead to fatigue, low blood sugar, and an impaired stress response. Similarly, a lack of aldosterone disrupts sodium and potassium balance, leading to low blood pressure and dehydration.
Causes of Addison’s Disease
Addison’s disease occurs when the adrenal glands are damaged due to the following causes:
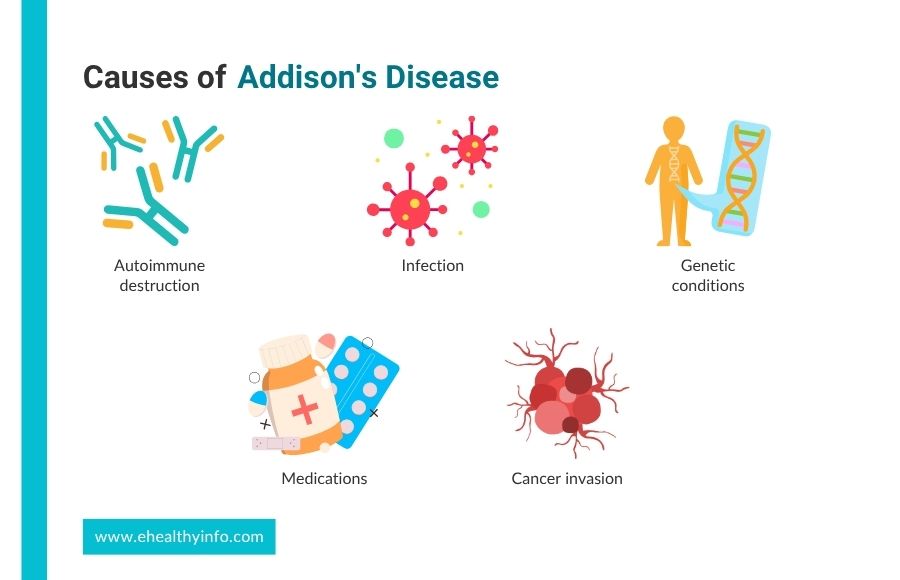
1. Autoimmune Destruction
The most common cause is autoimmune adrenalitis, an autoimmune disease where the immune system attacks the body’s cells and organs. In developed countries, autoimmune diseases cause eight or nine out of every 10 cases of Addison’s disease.
2. Infection
Tuberculosis (TB) used to be the most common cause, but better treatments have made TB a less frequent cause. People with HIV/AIDS are at risk because of their weakened immune systems.
3. Genetic Conditions
Genetic disorders affecting adrenal gland development or function. It can be part of genetic conditions like Autoimmune Polyglandular Syndrome Type 1 (APS1) and X-linked Adrenoleukodystrophy (X-ALD).
4. Medications
Certain medications can cause Addison’s disease by damaging the adrenal glands, blocking hormone production, or triggering an immune attack. Drugs like ipilimumab, nivolumab, pembrolizumab, ketoconazole, fluconazole, etomidate, rifampicin, and warfarin can all lead to adrenal insufficiency through various mechanisms.
5. Other Causes
Other less common causes of Addison’s disease include cancer cells in the adrenal glands, surgical removal of the adrenal glands, and bleeding into the adrenal glands.
Symptoms of Addison’s Disease
The symptoms of Addison’s Disease can develop slowly and may include:

1. Weakness
Low cortisol reduces glucose production and storage, leading to low energy and blood pressure. You might feel very tired and weak, even if you sleep well. This tiredness can make it hard for you to do your daily activities and may leave you feeling worn out with little effort.
2. Weight Loss
Intentional weight loss is a hallmark of Addison’s disease. The body’s metabolism is disrupted due to insufficient cortisol, leading to reduced appetite and fat loss. In some cases, muscle mass may also decrease.
3. Darkening of the Skin
Your skin might start to look darker, especially in areas exposed to the sun, around scars, and on the creases of your hands. This happens because your body produces more melanin, the pigment that colors your skin.
4. Low Blood Pressure
Aldosterone regulates sodium and water balance in the body. Low aldosterone levels cause the body to lose sodium and water, leading to low blood pressure. This can result in dizziness, especially when standing up, and you may even feel lightheaded.
5. Salt Craving
You may find yourself wanting salty foods more than usual. This craving is a response of your body as the body attempts to replenish sodium levels, which are essential for maintaining blood pressure and fluid balance.
6. Low Blood Sugar
Cortisol helps maintain normal blood sugar levels, particularly during stress or fasting. A lack of cortisol leads to low blood sugar, which can cause symptoms such as shakiness, sweating, confusion, and fainting.
7. Nausea and Vomiting
You could feel sick to your stomach or even throw up, sometimes with stomach pain. These issues are common with Addison’s Disease and can make it hard to eat and stay nourished.
Addisonian Crisis
An Addisonian crisis, or adrenal crisis, is a life-threatening condition that occurs when your body’s cortisol levels. It is often triggered by stress like infection, surgery, trauma, or severe vomiting and diarrhea. Symptoms of an adrenal crisis include severe weakness, low blood pressure, vomiting, diarrhea, dehydration, confusion, and loss of consciousness. If left untreated, it can lead to shock, organ failure, or even death.
Diagnosis of Addison’s Disease
Diagnosis of Addison’s disease involves several steps to confirm adrenal insufficiency and identify the underlying cause.

Blood Tests
Blood tests are crucial for diagnosing Addison’s disease and include checking for:
- Cortisol levels: Cortisol is the primary hormone affected in Addison’s disease. Low cortisol levels, especially in the morning when levels are typically highest, can suggest adrenal insufficiency.
- Adrenocorticotropic hormone (ACTH): It is a hormone produced by the pituitary gland and stimulates the adrenal glands to produce cortisol. In Addison’s disease, ACTH levels are often elevated as the body tries to signal the adrenal glands to produce more cortisol.
- Sodium and potassium levels: Due to aldosterone deficiency, low sodium, and high potassium levels are common in Addison’s disease.
- Renin and aldosterone levels: Renin is a hormone the kidneys produce to regulate blood pressure. In Addison’s disease, renin levels may be elevated, while aldosterone levels are typically low, indicating a dysfunction in adrenal hormone production.
ACTH Stimulation Test
This is one of the most definitive tests for Addison’s disease. A synthetic form of ACTH is injected into the patient, and cortisol levels are measured before and after the injection. In healthy individuals, the adrenal glands should respond by producing more cortisol. In Addison’s disease, the cortisol levels either remain low or show only a minimal increase, indicating impaired adrenal function.
Imaging Tests
- Computed Tomography (CT): A CT scan of the abdomen can help identify if the adrenal glands are damaged, shrunken, or affected by other conditions like infections, tumors, or hemorrhage.
- Magnetic Resonance Imaging (MRI): Sometimes, if the cause of adrenal insufficiency is suspected to be secondary due to pituitary dysfunction, an MRI scan of the brain may be done to assess the pituitary gland.
Autoimmune Antibody Tests
Since Addison’s disease is often caused by an autoimmune attack on the adrenal glands, testing for certain antibodies (such as anti-21-hydroxylase antibodies) can help confirm an autoimmune cause.
Treatment of Addison’s Disease
Treatment for Addison’s Disease involves lifelong replacement of the hormones your adrenal glands aren’t making.
Hormone Replacement Therapy
1. Glucocorticoid Replacement
The primary treatment for Addison’s disease is to replace the missing cortisol with a synthetic corticosteroid. Hydrocortisone is the most commonly prescribed medication, taken orally one to two times a day. It mimics your body’s natural cortisol production. Depending on the patient’s response and preferences, Prednisone or Dexamethasone may be used as an alternative.
2. Aldosterone Replacement
Fludrocortisone is the medication that helps maintain sodium balance, but you need to monitor your salt intake carefully.
3. Adrenal Androgen Replacement
Dehydroepiandrosterone (DHEA) supplementation may improve your quality of life.
Stress Dosing for Illness or Surgery
You need to adjust your steroid doses during physical stress, such as illness, injury, or surgery. The body naturally produces more cortisol during stress, but in Addison’s disease, you can’t respond adequately as other people. So, you might need to increase the hydrocortisone dose to prevent adrenal crisis. Many people are also advised to carry a self-injection kit of hydrocortisone in case of severe illness or injury.
Managing an Adrenal Crisis
The first step in the management of an adrenal crisis is intravenous hydrocortisone. It helps to replace the cortisol that your body cannot produce quickly. You also need intravenous fluids to treat dehydration, correct low blood pressure, and electrolyte replacement to address imbalances like low sodium and high potassium. Sometimes, your glucose level may become very low, which might need to be added to your fluid.
Tips for People living with Addison’s Disease
Living with Addison’s disease requires careful management, but with the right approach, individuals can lead healthy lives. Here are some essential tips:
1. Medication Adherence
Taking prescribed corticosteroid medications daily is crucial to replace missing hormones. Missing doses can lead to severe complications like adrenal crises.
2. Carry Emergency Kit
Always have an emergency hydrocortisone injection kit on hand, especially during travel or stressful situations. This can be life-saving during an adrenal crisis.
3. Recognize Warning Signs
You should learn to recognize early symptoms of an adrenal crisis, such as severe fatigue, dizziness, vomiting, or confusion, and seek immediate medical help.
4. Stress Management
Stress can trigger an adrenal crisis, so it’s important to manage it through relaxation techniques like meditation or yoga.
5. Maintain Regular Check-Ups
Regular doctor visits are necessary to monitor hormone levels and adjust medications as needed.
6. Wear Medical Alert ID
A medical alert bracelet or necklace informs healthcare providers of your condition in emergencies when you cannot communicate.
Dietary Recommendations
To manage Addison’s disease, focus on dietary adjustments that address your specific needs.

1. Electrolyte Balance
Increase your sodium intake to compensate for sodium loss due to aldosterone deficiency. This is especially important in hot weather or during heavy sweating. Monitor your potassium levels, as you may need to keep an eye on them, particularly if you have issues with high potassium.
2. Prevention of Hypoglycemia
Eat regular, balanced meals with complex carbohydrates, proteins, and healthy fats to keep your blood sugar stable overnight. You can try eating uncooked cornstarch before bed, which slowly releases glucose. You might also snack on fruits, glucose tablets, or drinks with glucose. Complex carbs with protein, like whole grain crackers with cheese or a peanut butter sandwich, help maintain steady glucose levels. Nuts like almonds or pistachios are also good for keeping your energy up.
3. Bone Health
Ensure you get enough calcium and vitamin D to support bone health, as you are at risk for osteoporosis. You can get these nutrients through your diet or supplements if needed.
4. General Nutritional Support
Maintain a balanced diet with plenty of fruits, vegetables, lean proteins, and whole grains to support overall health. Also, drink plenty of fluids to prevent dehydration, which can worsen your symptoms.
Addison’s Disease and Vitiligo
Addison’s disease and Vitiligo are often linked because both involve autoimmune attacks. In vitiligo, the immune system destroys melanocytes, causing skin to lose color. In Addison’s disease, it attacks the adrenal glands, leading to low levels of cortisol and aldosterone.
If you have vitiligo, it’s important to watch for symptoms of Addison’s disease, such as fatigue, low blood pressure, and electrolyte imbalances. Early detection and treatment of Addison’s disease can help prevent severe complications
President of the United States and Addison’s Disease
John F. Kennedy, the youngest person ever elected President of the United States, was diagnosed with Addison’s disease in 1947 at the age of 30 while he was in London. Although he had this condition and other autoimmune diseases, JFK kept them a secret during his time in office. He was tragically assassinated on November 22, 1963, while campaigning for re-election, and his full medical history wasn’t revealed until years later. Today, Addison’s Disease Day is celebrated on May 29, President Kennedy’s birthday.
Questions To Ask Your Doctor
- What activities can trigger my symptoms?
- How will I know if my condition is getting worse, and what should I do?
- What should I do if I miss a dose of my medication?
- Are there any support groups or resources for people living with Addison’s disease?
- How can I manage fatigue and low energy levels on a day-to-day basis?
References
- Autoimmune Addison disease: MedlinePlus Genetics [Internet]. medlineplus.gov. Available from: https://medlineplus.gov/genetics/condition/autoimmune-addison-disease/
- Munir S, Waseem M. Addison disease [Internet]. National Library of Medicine. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441994/
- Thau L, Gandhi J, Sharma S. Physiology, cortisol [Internet]. National Library of Medicine. StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538239/
- Scott JH, Menouar MA, Dunn RJ. Physiology, Aldosterone [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470339/#:~:text=Aldosterone%20causes%20sodium%20to%20be
- Dutt M, Wehrle CJ, Jialal I. Physiology, Adrenal Gland [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537260/#:~:text=The%20adrenal%20gland%20is%20made
- Husebye E, Løvås K. Pathogenesis of primary adrenal insufficiency. Best Practice & Research Clinical Endocrinology & Metabolism. 2009 Apr;23(2):147–57.
- Nassoro DD, Mkhoi ML, Sabi I, Meremo AJ, Lawala PS, Mwakyula IH. Adrenal Insufficiency: A Forgotten Diagnosis in HIV/AIDS Patients in Developing Countries. International Journal of Endocrinology [Internet]. 2019 Jun 23;2019:1–9. Available from: https://www.hindawi.com/journals/ije/2019/2342857/
- Alevritis EM, Sarubbi FA, Jordan RM, Peiris AN. Infectious Causes of Adrenal Insufficiency. Southern Medical Journal. 2003 Sep;96(9):888–90.
- Eriksson D, Røyrvik EC, Aranda-Guillén M, Berger AH, Landegren N, Artaza H, et al. GWAS for autoimmune Addison’s disease identifies multiple risk loci and highlights AIRE in disease susceptibility. Nature Communications. 2021 Feb 11;12(1).
- Barthel A, Benker G, Berens K, Diederich S, Manfras B, Gruber M, et al. An update on Addison’s disease. Experimental and Clinical Endocrinology & Diabetes [Internet]. 2019;127(02/03):165–75. Available from: https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0804-2715
- Soule S. Addison’s disease in Africa teaching hospital experience. Clinical Endocrinology. 1999 Jan;50(1):115–20.
- Jakobi JM, Killinger DW, Wolfe BM, Mahon JL, Rice CL. Quadriceps muscle function and fatigue in women with Addison’s disease. Muscle & Nerve. 2001;24(8):1040–9.
- ADAMS R, KAYHINKEBEIN M, McQUILLEN M, SUTHERLAND S, ASYOUTY SE, LIPPMANN S. Prompt Differentiation of Addisonʼs Disease From Anorexia Nervosa During Weight Loss and Vomiting. Southern Medical Journal. 1998 Feb;91(2):208–11.
- Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and Treatment of Primary Adrenal Insufficiency: an Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism. 2016 Feb;101(2):364–89.
- Liamis G, Milionis HJ, Elisaf M. Endocrine disorders: Causes of hyponatremia not to neglect. Annals of Medicine. 2010 Oct 22;43(3):179–87.
- Kemp WL, Koponen MA, Meyers SE. Addison Disease: The First Presentation of the Condition May be at Autopsy. Academic Forensic Pathology [Internet]. 2016 Jun 1 [cited 2020 May 8];6(2):249–57. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31239896
- Meyer G, Hackemann A, Reusch J, Badenhoop K. Nocturnal Hypoglycemia Identified by a Continuous Glucose Monitoring System in Patients with Primary Adrenal Insufficiency (Addison’s Disease). Diabetes Technology & Therapeutics [Internet]. 2012 May 1 [cited 2021 Jan 19];14(5):386–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3338953/#__ffn_sectitle
- Meyer G, Badenhoop K. [Addisonian Crisis – Risk Assessment and Appropriate Treatment]. Deutsche Medizinische Wochenschrift (1946) [Internet]. 2018 Mar 1;143(6):392–6. Available from: https://pubmed.ncbi.nlm.nih.gov/29544234/
- Al-Aridi R, Abdelmannan D, Arafah B. Biochemical Diagnosis of Adrenal Insufficiency: The Added Value of Dehydroepiandrosterone Sulfate Measurements. Endocrine Practice. 2011 Mar;17(2):261–70.
- Ospina NS, Al Nofal A, Bancos I, Javed A, Benkhadra K, Kapoor E, et al. ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis. J Clin Endocrinol Metab 2016;101:427–34. https://doi.org/10.1210/jc.2015-1700.
- Winters SJ, Vitaz T, Nowacki MR, Craddock DC, Silverman C, Lopez FA. Addison’s Disease and Pituitary Enlargement. Am J Med Sci 2015;349:526–9. https://doi.org/10.1097/MAJ.0000000000000305.
- Oelkers W, Diederich S, Bähr V. Diagnosis and therapy surveillance in Addison’s disease: rapid adrenocorticotropin (ACTH) test and measurement of plasma ACTH, renin activity, and aldosterone. The Journal of Clinical Endocrinology & Metabolism. 1992 Jul;75(1):259–64.
- Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2016;101:364–89. https://doi.org/10.1210/jc.2015-1710.
- Løvås K, Husebye ES. Replacement therapy in Addison’s disease. Expert Opin Pharmacother 2003;4:2145–9. https://doi.org/10.1517/14656566.4.12.2145
- Napier C, Pearce SHS. Current and emerging therapies for Addison’s disease. Curr Opin Endocrinol Diabetes Obes 2014;21:147–53. https://doi.org/10.1097/MED.0000000000000067.
- Schöfl C, Mayr B, Maison N, Beuschlein F, Meyer G, Badenhoop K, et al. Daily adjustment of glucocorticoids by patients with adrenal insufficiency. Clin Endocrinol (Oxf) 2019;91:256–62. https://doi.org/10.1111/cen.14004
- Prete A, Taylor AE, Bancos I, Smith DJ, Foster MA, Kohler S, et al. Prevention of Adrenal Crisis: Cortisol Responses to Major Stress Compared to Stress Dose Hydrocortisone Delivery. J Clin Endocrinol Metab 2020;105:2262–74. https://doi.org/10.1210/clinem/dgaa133.
- Petersen KS, Rushworth RL, Clifton PM, Torpy DJ. Recurrent nocturnal hypoglycaemia as a cause of morning fatigue in treated Addison’s disease – favourable response to dietary management: a case report. BMC Endocr Disord 2015;15:61. https://doi.org/10.1186/s12902-015-0058-6.
- Lee P, Greenfield JR. What is the optimal bone‐preserving strategy for patients with <scp>A</scp> ddison’s disease? Clin Endocrinol (Oxf) 2015;83:157–61. https://doi.org/10.1111/cen.12730.
- Kemp EH, Waterman EA, Weetman AP. Immunological pathomechanisms in vitiligo. Expert Rev Mol Med 2001;3:1–22. https://doi.org/10.1017/S1462399401003362.
- Boniface K, Seneschal J, Picardo M, Taïeb A. Vitiligo: Focus on Clinical Aspects, Immunopathogenesis, and Therapy. Clin Rev Allergy Immunol 2018;54:52–67. https://doi.org/10.1007/s12016-017-8622-7.
Return to Home
