Anticoagulants – Apixaban, Rivaroxaban, Warfarin, and Blood Thinner Medication

| Highlights on Anticoagulants
- Anticoagulants increase the risk of bleeding, which might show up as more bruising, nosebleeds, bleeding gums, pink or brown urine, or heavier menstrual periods.
- Contact sports can increase your chance of bleeding, so wear protective sportswear to protect yourself from injuries while on anticoagulation.
- Pregnancy is one of the conditions where you may require anticoagulants. However, it requires careful monitoring due to potential harm to the baby.
- If you are on warfarin, maintaining a consistent intake of vitamin K-rich foods is essential to avoid fluctuations in INR levels.
- Newer anticoagulants like Eliquis, Xarelto, and Pradaxa do not need regular monitoring with INR.
What are Anticoagulants?
Anticoagulants are medicines that slow down the clotting process in your blood. Although they’re sometimes called “blood thinners, ” they don’t really thin blood. Instead, these medications either break down existing clots or prevent new ones from forming in your heart, veins, and arteries.
Anticoagulants are available in different forms. Some come in pills. Others are given to you as a shot or through the intravenous route. They’re often used to treat and prevent serious conditions caused by blood clots, like stroke, heart attacks, and pulmonary embolisms. [1]
Why Might Someone Need To Take Anticoagulants?
When blood clots form at the right place to heal an injury, they are helpful. But if they move around in your bloodstream, they can be very dangerous. A large clot can block a small blood vessel, stopping blood flow to an organ, which can be life-threatening. Anticoagulants are often prescribed for the following health conditions:
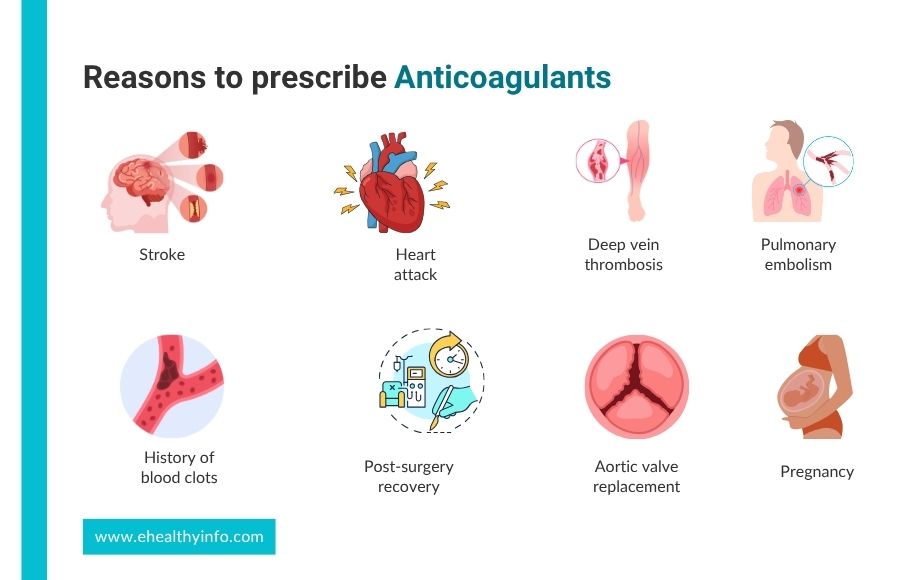
1. Stroke
A clot can block blood from flowing to your brain, damaging or killing brain cells, causing permanent damage or even death.
2. Transient ischemic attack (TIA)
These are like “mini-strokes” with similar symptoms to stroke but don’t last long, usually less than a day.
3. Heart attack
A clot can block a blood vessel in your heart, causing chest pain, and, in serious cases, death may result if your heart does not get enough oxygen.
4. Deep vein thrombosis (DVT)
Blood clots forming in your deep veins, often in the legs, can cause pain and swelling.
5. Pulmonary embolism
A blood clot blocking a blood vessel around your lungs can disrupt its blood supply and make you short of breath.
If you’re at risk of these clot-related events due to clotting problems or diseases, anticoagulants are recommended.
Additionally, they might be prescribed for individuals with:
- History of blood clots: If you have had clots, your doctor might suggest anticoagulants after checking what caused them and analyzing your risk factors for developing further ones.
- Post-surgery recovery: After hip or knee replacement surgery, you face a higher risk of clots forming in your leg veins. This condition, known as deep vein thrombosis, is a major cause of pulmonary embolism. To avoid this condition, anticoagulants are given prophylactically. [2]
- Aortic valve replacement: When your valves are replaced, these new valves can be the site of clot formation. Anticoagulants help in preventing this clot formation.
- Medical conditions: Certain conditions, like Factor V Leiden deficiency and antiphospholipid syndrome, affect blood clotting. Some of these conditions are genetic, which can be inherited from or passed to family members. These patients may require anticoagulant life long. [3]
- Pregnancy: Anticoagulants might be recommended in pregnancy, as they can increase the risk of blood clots by five times, and this risk can rise even further, to twenty times or more, after childbirth. [4]
How do Anticoagulants Work?
When you get a cut or injury, your body must form a clot to stop the bleeding. Thrombin is a substance that helps in making these clots. However, too much thrombin can sometimes be a problem, leading to excessive clot formation. Anticoagulants help by reducing the production of thrombin or blocking its activity, preventing unwanted blood clotting.
Some anticoagulants, like warfarin, work by interfering with vitamin K, which is needed for thrombin production. Others, like heparin, target a substance called factor Xa to prevent thrombin formation. Dabigatran is another anticoagulant that directly blocks thrombin formation. Overall, these medications help prevent the formation of dangerous blood clots, ultimately reducing your risk of having serious health problems like strokes or heart attacks.
Types of Anticoagulants
There are three main types of anticoagulant drugs:
- Vitamin K antagonists
- Direct Oral Anticoagulants (DOACs)
- Low molecular weight heparins (LMWH)
1. Vitamin K antagonist
Warfarin, commonly known as Coumadin, is a pill you take once a day by mouth. It works by stopping an enzyme that activates vitamin K, which is important for making substances that help your blood clot.
While warfarin can be very helpful for those who need it, it also raises the risk of bleeding. That is why it is important to have regular blood tests to make sure you are taking the right amount. It is not safe to take warfarin if you are pregnant because it can harm the baby. However, if you’re breastfeeding, you can usually take warfarin without any issues. Also, it won’t affect your ability to have children in the future.[5]
2. Direct Oral Anticoagulants (DOACs)
DOACs work faster than older anticoagulants like warfarin. Studies have shown that DOACs may lead to less bleeding than other anticoagulants like warfarin and are often more predictable. DOACs are easier for you to take because their dosing is simpler, and they are less affected by what you eat and other medications you might be taking. DOACs include:
- Direct thrombin inhibitors: As their name suggests, these drugs interfere with thrombin directly. Although they are typically administered through injections, they are also available in pill form, like dabigatran (Pradaxa).
- Direct factor Xa inhibitors: These anticoagulants prevent factor Xa, an important part of the clotting process. They come in pill form and include drugs like apixaban (Eliquis), edoxaban (Savaysa), dabigatran (Pradaxa), and rivaroxaban (Xarelto).
With these medications, you don’t need regular blood tests to monitor your clotting function. Instead, you will have a blood test every 6 to 12 months to monitor your kidney function. [6] If you forget to take a dose, take it as soon as you remember. Then, continue with your regular schedule the next day. But if it is nearly time for your next dose, do not take the missed one and continue with your normal schedule. You must avoid taking two doses simultaneously to compensate for the missed one.
3. Low Molecular Weight Heparin (LMWH)
LMWH is an injection commonly used temporarily alongside oral anticoagulants like warfarin. It’s important to let your doctor know if you’re taking any nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin, ibuprofen, or naproxen, as they can increase your risk of bleeding when taken with heparin.
LMWH stays in your body longer, so you won’t need to visit the hospital as frequently for injections, and you won’t need regular blood tests. However, it may be more expensive, and getting the injections might be uncomfortable, especially if you’re afraid of needles. Also, it can be harder to reverse its effects if needed. There are no specific food restrictions with LMWH, but your doctor might recommend calcium and vitamin D supplements to protect your bones if you’re using them for an extended period.
Side Effects of Anticoagulants
Knowing when to seek emergency help is crucial for anyone taking blood thinners. Common side effects of anticoagulants are:

1. Bleeding
Any anticoagulants can put you at a greater risk of bleeding. You can have minor bleeding like bruising, nosebleeds that last longer than usual, bleeding gums, or prolonged bleeding from cuts. Sometimes, the bleeding can be more serious and include internal bleeding called major bleeding. This includes gastrointestinal bleeding, intracranial bleeding, and severe bleeding that requires medical attention or hospitalization. [7]
2. Warfarin
Apart from the risk of bleeding, warfarin can cause other side effects, like skin necrosis. It is one of the rare but serious complications that typically occur within the first few days of starting the therapy. It appears as painful, reddish-purple patches on the skin and can rapidly progress to blackened, necrotic tissue areas. This is due to the temporary imbalance between procoagulant and anticoagulant factors, as warfarin inhibits vitamin-K-dependent clotting factors. Other side effects of warfarin include purple toe syndrome, calciphylaxis, stomach pain, and changes in your sense of taste. [8]
3. LMWH
It can cause a serious condition called heparin-induced thrombocytopenia (HIT). HIT is a severe immune-mediated condition that leads to a paradoxical increase in clotting risk due to lower platelet count. HIT usually occurs after five days of starting heparin therapy and can lead to dangerous blood clots, increasing your risk of having complications such as pulmonary embolism, deep vein thrombosis, stroke, heart attack, and blockages in your major arteries. With heparin, you may experience injection-site reactions such as redness, swelling, or pain. Long-term use of LMWH can lead to other side effects like high potassium levels in your blood, hair loss, and weakening of your bones (osteoporosis). [9]
When To Seek Emergency Help When You’re on Anticoagulants?
Anticoagulants, commonly known as blood thinners, are vital for preventing blood clots. However, they can also pose significant risks. Knowing when to seek emergency help is crucial for anyone taking these medications. Here’s a comprehensive guide to help you understand when to take action.

When taking anticoagulants, it is important to seek medical help immediately if you experience signs of serious bleeding, such as prolonged or heavy bleeding from cuts, unusual or unexplained bruising, blood in urine or stool, blood in your cough, or vomit that looks like coffee grounds. Additionally, symptoms of internal bleeding, like severe headache, dizziness, weakness, unusual pain or swelling, and shortness of breath, require urgent medical attention. You should seek help if you have signs of a stroke, including sudden weakness, especially on one side of the body, difficulty speaking, confusion, or sudden vision problems. Also, report reactions such as itching, rash, swelling, trouble breathing, or severe dizziness.
International Normalized Ratio (INR)- What does it Mean?
INR is a test to check how well the blood-thinning medication warfarin (Coumadin®) works. It’s calculated from another test called the Prothrombin Time (PT). These tests help doctors see if warfarin is preventing blood clots effectively. The longer it takes the blood to clot in the assay, the higher the PT and INR. The target INR range depends on your specific medical situation. Usually, the target range is between 2 and 3, but sometimes different ranges may be chosen depending on special circumstances. If someone is not taking warfarin, the INR typically averages around one. [10]
If your INR is below the target range, you’re not getting enough blood thinning effect, and there’s a higher risk of clotting. If your INR is above the target range, it means you’re getting too much blood thinning effect, and there’s a higher risk of bleeding.
Monitoring of Anticoagulants
Monitoring anticoagulants is essential to ensure their effectiveness while decreasing the risk of adverse effects, especially bleeding. Regular blood tests to measure the INR are important for patients on warfarin, with the target INR range varying depending on the condition being treated. Patients on LMWH may require periodic monitoring of renal function and platelet counts to detect HIT and adjust dosages appropriately, especially in those with renal impairment. Newer oral anticoagulants, DOACs, generally require less frequent monitoring but still require periodic kidney and liver function tests. [11]
Tips for Preventing Excessive Bleeding while Taking Anticoagulants
To prevent bleeding while taking anticoagulants, it’s important to be cautious during activities that could lead to injury, cuts, or bruises. Here are some tips to help:

- Avoid contact sports like football, rugby, hockey, and horse riding.
- Use gloves when handling sharp objects such as scissors, knives, or gardening tools.
- Instead of wet shaving or waxing, use an electric razor or hair-removing cream to prevent cuts.
- Take out dentures or retainers for a few hours daily to rest your gums and ensure they fit well to avoid irritation.
- Before any medical or dental procedures, including vaccinations and routine dental appointments, let your doctor, dentist, or nurse know you are taking anticoagulants. [12]
Foods, Supplements, and Drugs That Interact with Anticoagulants
When taking anticoagulants, it’s important to inform your healthcare team about any other medications or foods you’re taking or eating, such as supplements, natural medicines, vitamins, or alternative therapies. These can all affect how well your medication works.
1. Foods
Some foods, especially those high in vitamin K (broccoli, spinach, kale, and Brussels sprouts), cranberries, alcohol, soya beans, and canola oil, can impact how well your anticoagulant (such as warfarin) works. If you are on warfarin, maintaining a consistent intake of vitamin K-rich foods is essential to avoid fluctuations in INR levels. Alcohol, cranberry juice, and grapefruit juice should be limited due to their potential to increase bleeding risk. But if you take newer anticoagulants like rivaroxaban, dabigatran, apixaban, or edoxaban, you have fewer dietary interactions but still require careful monitoring. [13]
2. Drugs
Medications can significantly interact with anticoagulants, affecting their efficacy and safety. NSAIDs, such as ibuprofen and aspirin, can increase the risk of gastrointestinal bleeding when taken with anticoagulants. Certain antibiotics, like ciprofloxacin and metronidazole, can enhance the effects of warfarin, raising the risk of bleeding and necessitating close INR monitoring and potential dosage adjustments. Selective serotonin reuptake inhibitors (SSRIs) and other antidepressants can also increase bleeding risk. [14]
3. Supplements
Herbal supplements like ginkgo biloba, garlic, and St. John’s wort may alter the anticoagulant’s effects, either by increasing bleeding risk or reducing efficacy. Fish oil supplements can enhance the anticoagulant effect, increasing the risk of bleeding. Vitamin E supplements may have a similar effect, potentiating bleeding risk. [13]
When Should Anticoagulants be Avoided?
Anticoagulants should be avoided or used with extreme caution in certain situations to prevent potential complications. Contraindications to anticoagulant therapy include
- Active bleeding disorders,
- Recent major surgery,
- Severe liver disease,
- Severe thrombocytopenia and
- Uncontrolled hypertension.
Additionally, individuals with a history of intracranial bleeding, recent stroke, or certain types of gastrointestinal bleeding may not be suitable candidates for anticoagulant therapy. Pregnancy and breastfeeding also require careful consideration, as some anticoagulants can pose risks to the developing fetus or nursing infant. Patients with a known hypersensitivity to anticoagulant medications or any of their components should avoid their use. However, if the benefit of using anticoagulants outweighs the risk, your doctor may prescribe them.
Pregnancy and Anticoagulants
Pregnancy is known as a state of hypercoagulability, and women are likely to develop blood clots both during and after giving birth. If you need to take anticoagulants during pregnancy, your doctor will prescribe them very cautiously because these medications can harm the baby. However, it is very challenging to determine the right dosage during pregnancy. In addition, if you are someone who takes these medications regularly and wants to have a baby, you’ll need advice on how to keep the baby safe from the medicine’s effects and what to do during childbirth. [15]
Questions To Ask Your Doctor
- Will I require regular blood tests while on the anticoagulant you’re prescribing?
- What should I do if I have another clotting event while taking this medication?
- Can you explain how home monitoring for Warfarin works?
- Is it true that anticoagulants can make me more prone to sunburn?
- Can anticoagulants make me feel colder?
- Do I need to change my birth control while taking anticoagulants?
References
- Heestermans M, Poenou G, Hamzeh-Cognasse H, Cognasse F, Bertoletti L. Anticoagulants: A Short History, Their Mechanism of Action, Pharmacology, and Indications. Cells. 2022 Oct 13;11(20):3214. doi: 10.3390/cells11203214. PMID: 36291080; PMCID: PMC9600347.
- Jones A, Al-Horani RA. Venous Thromboembolism Prophylaxis in Major Orthopedic Surgeries and Factor XIa Inhibitors. Medical Sciences 2023;11(3):49.
- Kakkos SK, Gohel M, Baekgaard N, Bauersachs R, Bellmunt-Montoya S, Black SA, et al. Editor’s Choice – European Society for Vascular Surgery (ESVS) 2021 Clinical Practice Guidelines on the Management of Venous Thrombosis. European Journal of Vascular and Endovascular Surgery 2021;61(1):9–82.
- Marshall AL. Diagnosis, treatment, and prevention of venous thromboembolism in pregnancy. Postgrad Med. 2014 Nov;126(7):25-34. doi: 10.3810/pgm.2014.11.2830. PMID: 25387211.
- Bates SM, Rajasekhar A, Middeldorp S, McLintock C, Rodger MA, James AH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv 2018;2(22):3317–59.
- Burnett AE, Mahan CE, Vazquez SR, Oertel LB, Garcia DA, Ansell J. Guidance for the practical management of the direct oral anticoagulants (DOACs) in VTE treatment. J Thromb Thrombolysis. 2016 Jan;41(1):206-32. doi: 10.1007/s11239-015-1310-7. PMID: 26780747; PMCID: PMC4715848.
- Piran S, Schulman S. Treatment of bleeding complications in patients on anticoagulant therapy. Blood 2019;133(5):425–35.
- Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G. Oral Anticoagulant Therapy. Chest 2012;141(2):e44S-e88S.
- Warnock LB, Huang D. Heparin [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538247/
- Papala M, Gillard D, Hardman J, Romano T, Rein LE. Extending INR testing intervals in warfarin patients at a multi-center anticoagulation clinic. J Thromb Thrombolysis 2022;53(3):626–32.
- Conway SE, Hwang AY, Ponte CD, Gums JG. Laboratory and Clinical Monitoring of Direct Acting Oral Anticoagulants: What Clinicians Need to Know. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy 2017;37(2):236–48.
- Anticoagulants [Internet]. Heart and Stroke Foundation of Canada. Available from: https://www.heartandstroke.ca/heart-disease/treatments/medications/anticoagulants
- Tan CSS, Lee SWH. Warfarin and food, herbal or dietary supplement interactions: A systematic review. Br J Clin Pharmacol 2021;87(2):352–74.
- Mar PL, Gopinathannair R, Gengler BE, Chung MK, Perez A, Dukes J, et al. Drug Interactions Affecting Oral Anticoagulant Use. Circ Arrhythm Electrophysiol 2022;15(6).
- Alshawabkeh L, Economy KE, Valente AM. Anticoagulation During Pregnancy. Journal of the American College of Cardiology [Internet]. 2016 Oct [cited 2020 Jan 15];68(16):1804–13. Available from: http://www.onlinejacc.org/content/68/16/1804
Return to Home
