
Atopic dermatitis, also known as atopic eczema, is a condition that causes the skin to become dry, itchy, and inflamed. Atopic dermatitis is the most common chronic inflammatory skin disease. It usually begins in infancy or childhood but can develop at any age. [1]
There are many different types of atopic dermatitis. The most common ones are:
This is the most common form, often starting in childhood. It causes dry, itchy, and inflamed skin, usually on the face, elbows, and knees. [2]
This occurs when your skin reacts to allergens or irritants like soaps, fragrances, or metals. It causes redness, itching, and sometimes blisters. [3]
This type affects oily areas like the scalp, face, and chest, causing redness, scaling, and dandruff-like flakes. It is linked to yeast overgrowth and genetics. [4]
This type appears as round, coin-shaped patches of irritated skin, often after skin injuries like cuts or insect bites. It is more common in adults. [5]
Atopic dermatitis happens due to a mix of genetics, immune system issues, and environmental factors.
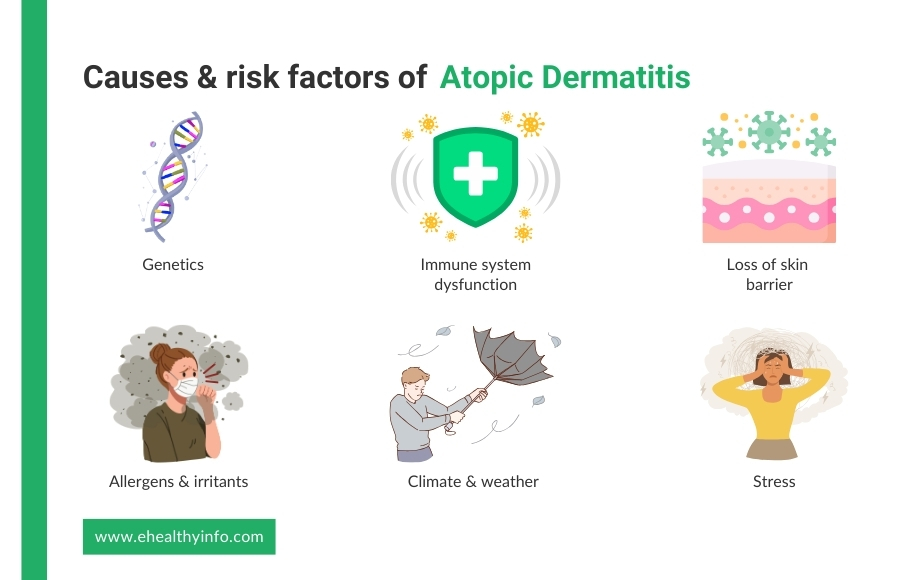
If your family has a history of eczema, asthma, or allergies, you will likely develop atopic dermatitis. If one parent has atopic dermatitis, your risk of developing it is 50%, increasing to 80% if both parents are affected. Similarly, a gene mutation can compromise your skin barrier, leading to dryness and increased sensitivity to irritation. [6]
Your immune system may overreact to harmless substances, leading to inflammation, redness, and itching. [7]
A weak skin barrier allows moisture to escape and irritants, allergens, and bacteria to enter, making your skin dry and easily inflamed. [6]
Pollen, dust mites, pet dander, soaps, and fragrances can trigger flare-ups by irritating your skin. [8]
Cold, dry air can worsen eczema by drying out your skin, while hot weather and sweating can cause itching and irritation. [6]
Emotional stress can trigger or worsen eczema by increasing inflammation in your body. [9]
People with atopic dermatitis may report periods with less marked symptoms followed by periods when symptoms are more severe, known as flare-ups. There may be various triggers that may lead to such flare-ups, such as strong soaps, detergents, skin care products, perfumes, makeup products, fabrics like wool or linen, pollen, mold, dust mites, animal dander, tobacco smoke, stress, anger, anxiety, low humidity, dry skin, sweating, or skin infections. [10]
The most common symptom of atopic dermatitis is itching. Other common symptoms include:
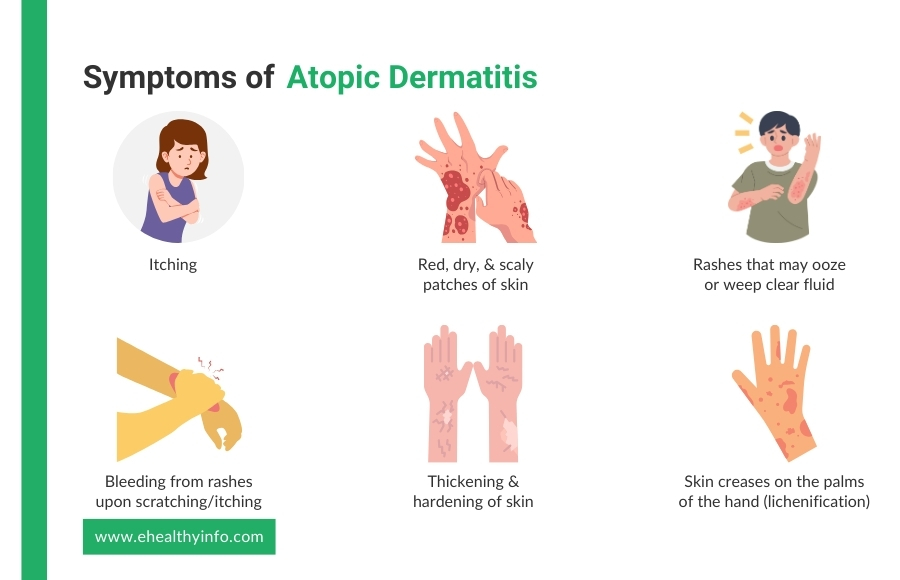
Atopic dermatitis usually starts with dry, itchy skin that becomes inflamed due to repeated scratching. In the early stages, the skin appears red and irritated and may have small bumps that ooze fluid. As the condition progresses, persistent scratching and rubbing cause the skin to thicken and become rough, a process called lichenification. This thickened skin develops deep lines, a leathery texture, and darker or lighter patches than the surrounding skin. Lichenified lesions are more resistant to treatment and can cause chronic itching and discomfort, often worsening in flare-ups. [11]
Examination of the lesion is the initial and the most important way to diagnose the conditions. You might need repeated examinations by your doctor to recognize the type of atopic dermatitis. Other tests that might be helpful to diagnose eczema are:
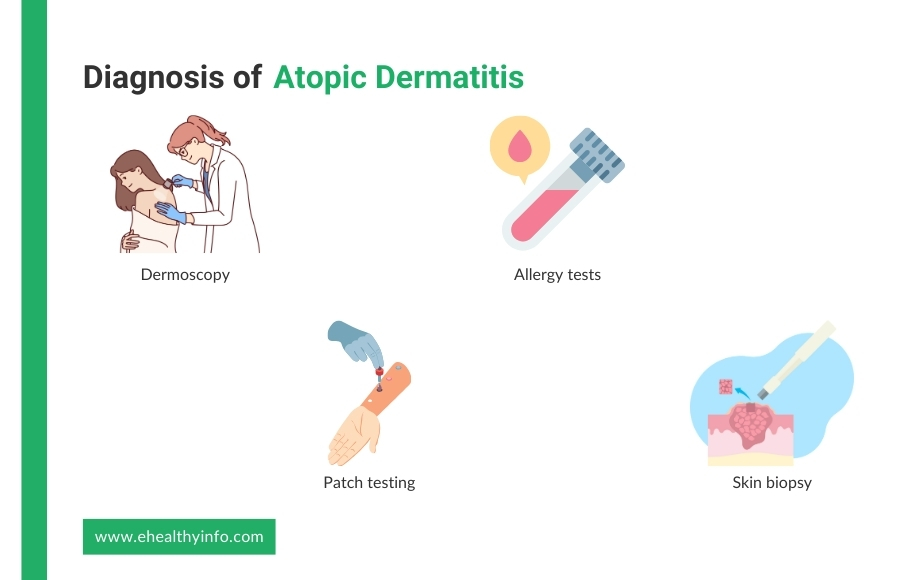
A dermoscopy is a tool your doctor may use to examine your skin closely. This handheld device magnifies the skin’s surface and helps the doctor identify patterns and small details that may not be visible to the naked eye. Dermoscopy can help distinguish atopic dermatitis from other skin conditions, ensuring an accurate diagnosis. [12]
Since atopic dermatitis can be triggered by allergens, your doctor might suggest allergy testing. Skin prick tests or blood tests can help identify environmental or food-related triggers that might worsen your symptoms, like pollen, dust, or certain foods. These tests can assist in managing flare-ups by avoiding triggers. [13]
Patch testing is a special allergy test that may be done if your doctor suspects that a contact allergen could trigger your symptoms. This test involves applying small amounts of different substances to your skin to see if any cause irritation or allergic reactions. It helps identify potential triggers that might be worsening your eczema. [14]
In some rare cases, a skin biopsy may be performed when the diagnosis is unclear. A small skin sample is removed and examined under a microscope to rule out other skin diseases with similar symptoms, such as psoriasis or contact dermatitis. [15]
Various treatment options are available, and the choice is made based on the type, stage, and severity of the condition.

One of the most important aspects of treating atopic dermatitis is regularly using moisturizers. These help lock moisture into your skin, which is key because dry skin can trigger or worsen flare-ups. Moisturizers come in different forms, such as creams, ointments, or lotions. Ointments are thicker and work better for severe dryness, while creams are lighter and can be used more frequently. It’s best to apply moisturizers right after bathing when your skin is still damp, as this helps to trap moisture in. Emollient-rich moisturizers can help create a protective barrier that reduces water loss and soothes irritated skin. [16]
Topical corticosteroids are often prescribed to reduce inflammation and itchiness. These medications are available in different strengths, from mild to potent, depending on the severity of the condition. You have to use them sparingly and only during flare-ups to avoid side effects like skin thinning. A milder steroid may be preferred for sensitive areas, like the face or groin. [17]
If your condition is severe or you need to use steroids for a very long period, topical calcineurin inhibitors, such as tacrolimus or pimecrolimus, can be your alternative. These medications help to control inflammation by inhibiting the immune system’s inflammatory response without the risks associated with steroids. They’re typically used in sensitive areas like the face or eyelids. [17]
For more severe cases of atopic dermatitis, doctors might prescribe oral medications, such as oral corticosteroids or immunosuppressive drugs like cyclosporine. These suppress the immune system’s overactive response and reduce inflammation. Systemic medications, however, are typically used as a last resort due to potential side effects. [18]
Since it is one of the most common symptoms of auto dermatitis, antihistamines are often recommended. They work by blocking histamine, a substance released by your immune system during an allergic reaction, which can cause itching. These can be helpful, especially at night, as they may also have a sedative effect to help with sleep when itching is severe. [17]
Phototherapy (or light therapy) involves exposing the skin to controlled amounts of ultraviolet (UV) light under medical supervision. This treatment can help reduce inflammation and improve symptoms, particularly in severe cases of atopic dermatitis that don’t respond to topical treatments. It’s commonly used in cases where the condition is widespread and persistent. [18]
Antibiotics are not needed for dermatitis, but with the cracks in the skin because of atopic dermatitis, there is a very high chance of infection. Atopic dermatitis is commonly associated with infections caused by Staphylococcus aureus. Managing these infections can help prevent the condition from worsening. [19]
Making lifestyle adjustments is crucial in managing atopic dermatitis. This includes avoiding known triggers like harsh soaps, certain fabrics (such as wool), and hot water. Using gentle, fragrance-free skin care products and wearing soft, breathable clothes can also help minimize irritation. Additionally, managing stress through relaxation techniques like meditation or yoga can prevent flare-ups since stress is a known trigger. [20]
People with atopic dermatitis may be more likely to develop other health conditions.