
| Key highlights
Benign prostatic hyperplasia (BPH) is also called prostate gland enlargement. It is one of the common conditions as men age and affects approximately 50% of men by age 50 and up to 80% of men in their 80s. The enlarged prostate in BPH squeezes or partially blocks the surrounding urethra, the tube that transports urine from the bladder out of the body. This enlargement of the prostate can lead to compression of the urethra, resulting in lower urinary tract symptoms (LUTS) such as increased frequency of urination, urgency, weak urinary stream, incomplete bladder emptying, and nocturia.
The prostate gland is a small gland located just below the bladder and in front of the rectum in men. The primary function of the prostate gland is to produce seminal fluid, which is responsible for nourishing and transporting sperm during ejaculation. The prostate gland surrounds the urethra, which is the tube that carries urine from the bladder out through the penis.
The pathophysiology of BPH involves hormonal changes, particularly an increase in dihydrotestosterone (DHT) levels within the prostate gland due to the action of 5-alpha-reductase. This hormone imbalance leads to abnormal growth and proliferation of glandular epithelial cells and stromal cells within the prostate, resulting in gland enlargement.
Additionally, alterations in smooth muscle tone and neurogenic factors within the prostate gland contribute to urinary symptoms associated with BPH.
BPH and Prostate Cancer are distinct conditions affecting the prostate gland in men. BPH involves the non-cancerous enlargement of the prostate gland due to hormonal changes and aging, leading to compression of the urethra and urinary. It is a common condition in older men but is generally not associated with an increased risk of prostate cancer. In contrast, prostate cancer is characterized by the abnormal growth of cancerous cells within the prostate gland, which can potentially spread to other parts of the body. Prostate cancer usually does not cause symptoms in its early stages but can present with urinary changes, blood in the urine or semen, and other systemic symptoms as it progresses. Unlike BPH, prostate cancer is a serious disease that requires early detection and appropriate treatment to prevent complications and improve outcomes.
BPH can cause a variety of signs and symptoms, and these symptoms typically develop gradually and can range from mild to severe, depending on the degree of prostate enlargement and the extent of urethral obstruction. Common signs and symptoms of BPH include:
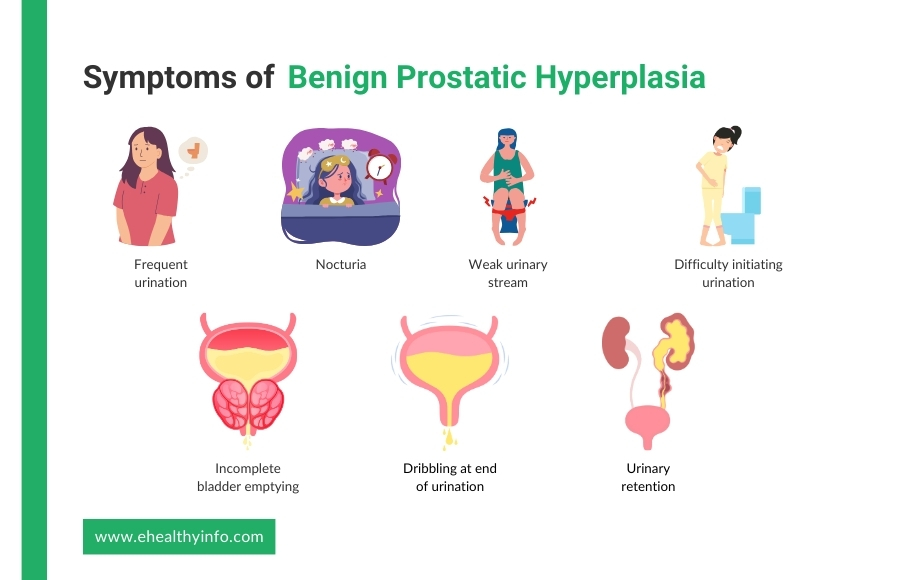
Men with BPH may experience a need to urinate more frequently, especially during the day.
You may have a sudden and strong urge to urinate, which can be difficult to postpone.
Men with BPH often experience nocturia. This refers to waking up during the night to urinate. This can be very disturbing to many as it disrupts your sleep patterns.
The urinary stream may be weak or diminished, making it difficult to start and complete urination.
You may have trouble starting the urine flow, requiring straining or pushing to begin urination.
Despite urinating, there may be a sensation of incomplete bladder emptying, leading to the need to urinate again shortly after.
After urination is complete, some men may experience dribbling or leakage of urine due to incomplete bladder emptying.
In severe cases of BPH, the urethra can become significantly obstructed, leading to urinary retention, where the bladder cannot empty completely. This is an emergency condition and requires urgent medical attention.
The diagnosis of BPH involves taking a medical history, performing a physical examination, and using various diagnostic tools. Here are the steps involved in the diagnosis:
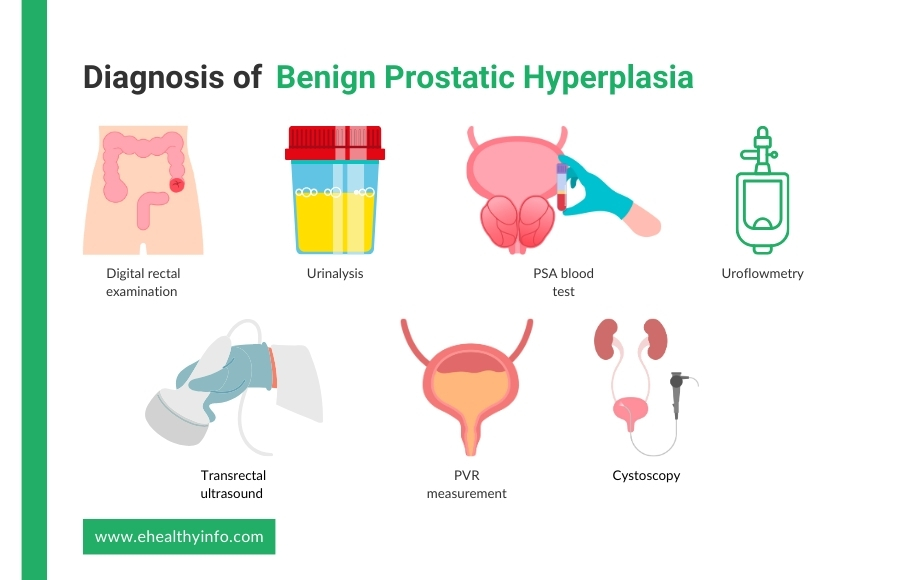
During a DRE, your doctor will insert a gloved, lubricated finger into the rectum to feel the size, shape, and consistency of the prostate gland. Enlargement, firmness, and nodules may indicate BPH or other prostate-related conditions.
A urinalysis may be performed to rule out other conditions, such as urinary tract infections or other abnormalities, contributing to the symptoms.
PSA is a protein produced by the prostate gland, and elevated levels can indicate BPH, prostate inflammation (prostatitis), or prostate cancer. The PSA test is used to assess prostate health and may help differentiate between BPH and prostate cancer.
Uroflowmetry is a non-invasive diagnostic test used to assess urinary function by measuring the rate and pattern of urine flow during voiding. During the procedure, you will be asked to urinate into a specialized toilet or uroflowmeter. The flow meter is equipped with sensors that record the flow electronically. It measures the parameters like the maximum flow rate, average flow rate, voided volume, and time to maximum flow. These measurements provide valuable information about urinary efficiency and can help diagnose conditions such as benign prostatic hyperplasia (BPH), urinary obstruction, or neurogenic bladder dysfunction.
Post-void residual urine measurement is an important diagnostic test for BPH and associated symptoms of LUTS. This test evaluates the amount of urine remaining in the bladder after urination, which can indicate inefficient bladder emptying due to BPH-related obstruction or other bladder abnormalities. Post-void residual urine can be measured using non-invasive methods such as bladder ultrasound (Bladder Scan) or inserting a catheter to drain and measure the residual urine volume directly. If you have BPH, you will have an elevated post-void residual volume.
In some cases, a TRUS may be performed to assess the size and structure of the prostate gland and rule out other conditions such as prostate cancer.
A cystoscopy is a procedure that involves inserting a thin, flexible tube into the urethra. The tube consists of a camera at the tip that helps to visualize the urinary tract. This may be recommended if there are concerns about bladder function or to rule out other urinary tract abnormalities.
You should know that there is no cure for BPH. However, treatment can manage your symptoms to some extent. The treatment of BPH aims to alleviate urinary symptoms, improve quality of life, and prevent complications. The treatment depends on the severity of your symptoms, the size of the prostate gland, the presence of complications, and individual patient preferences. Here are the main approaches to managing BPH:
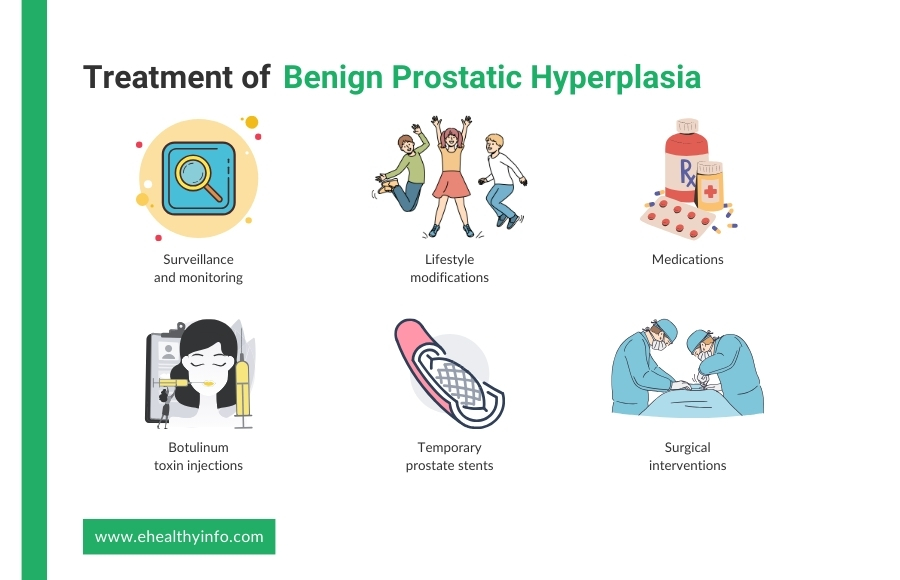
In cases of mild symptoms or when your symptoms are not bothersome, watchful waiting or active surveillance may be recommended. This involves regular monitoring of symptoms and prostate size without immediate treatment intervention.
Certain lifestyle changes can help manage mild to moderate symptoms of BPH. These include limiting fluid intake before bedtime, avoiding caffeine and alcohol, exercising regularly (especially pelvic floor exercises), and maintaining a healthy weight.
The use of medications is a common and effective approach for managing BPH, especially for individuals with moderate to severe symptoms. These medications primarily target the prostate gland and urinary tract to improve symptoms and reduce the obstruction caused by prostate enlargement.
Prostate surgery can have certain side effects and complications, including temporary urinary symptoms like urgency, frequency, or blood in urine immediately after surgery. Long-term effects may include erectile dysfunction, retrograde ejaculation, or urinary incontinence. Rare complications can include bleeding, urethral stricture (narrowing), bladder neck contracture, or persistent/recurrent symptoms. It’s prudent to discuss with your provider the side effects of prostate surgery before getting one.
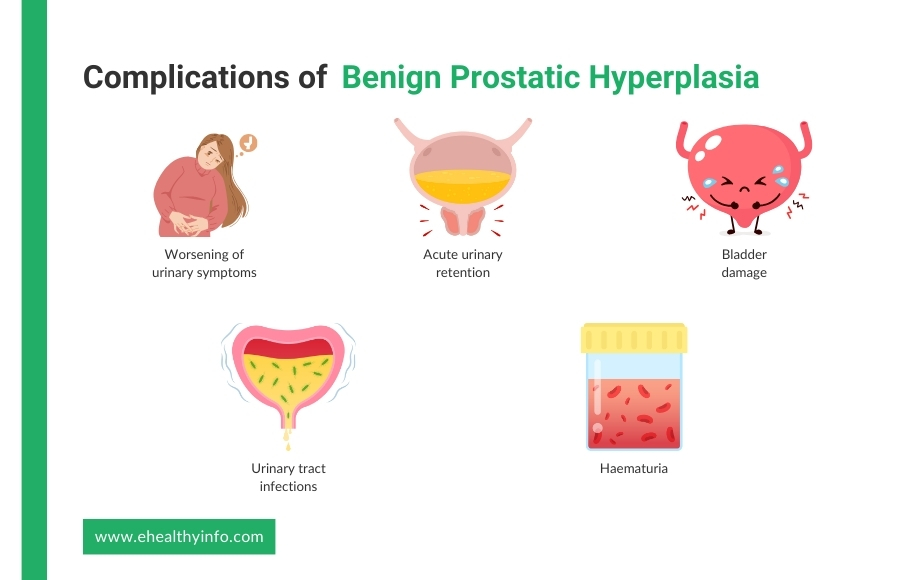
If BPH is left untreated, it can lead to various complications and progressively worsen over time. Some potential consequences of untreated BPH include:
There is no guaranteed way to avoid BPH.
However, decreasing weight and eating a well-balanced diet of fruits and vegetables may be beneficial. Excess body fat may raise hormone levels and other blood variables, stimulating the proliferation of prostate cells. Staying active aids in the management of weight and hormone levels.