Cardiomyopathy is a disease that affects the heart muscles, impairing their ability to pump blood to the rest of the body effectively. It often goes undetected, but it is estimated that approximately 1 in every 500 adults may have this condition. It can affect people of any age, sex, and race.
There are several types of cardiomyopathy; the common ones are as follows:
If you have hypertrophic cardiomyopathy, the muscular wall of your heart becomes thickened, making it difficult for your heart to pump blood effectively throughout your body. This condition is genetic, so if one of your parents has HCM, there is a 50 percent chance that you may have inherited HCM can develop at any age, but it tends to be more severe when it starts during childhood.
In dilated cardiomyopathy, the heart muscle becomes weakened and dilated, decreasing the heart’s ability to pump blood It is the most common type of cardiomyopathy.
Restrictive cardiomyopathy is a type of myopathy characterized by abnormal stiffness of the heart muscle, which impairs its ability to fill properly with blood during the relaxation phase of the heartbeat. This stiffness is often caused by infiltrating abnormal substances, such as scar tissue or proteins, into the heart muscle, which results in reduced ventricular filling and decreased cardiac output, leading to heart failure.
While the exact cause of cardiomyopathy is often complex and multifactorial, certain risk factors can increase the likelihood of developing this condition. Some of the risk factors are as follows:
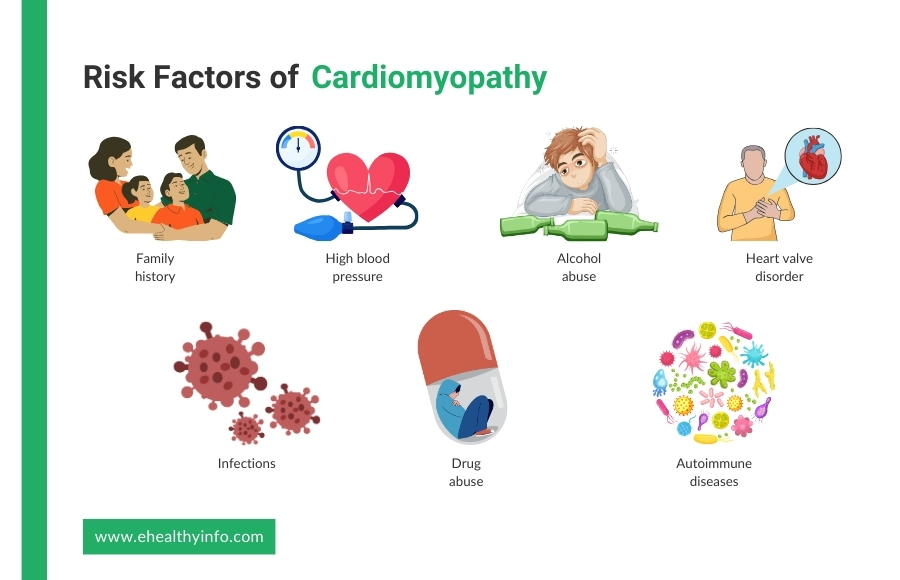
A family history of cardiomyopathy or sudden cardiac death can significantly increase the risk of developing the condition.
If you have uncontrolled high blood pressure, it can strain the heart muscle over time, leading to hypertensive cardiomyopaty. Hypertensive cardiomyopathy is a form of secondary cardiomyopathy characterized by thickening and stiffening of the heart muscle.
Excessive and prolonged drinking of alcohol can weaken the muscles in your heart and lead to the development of dilated cardiomyopathy.
Malfunctioning heart valves, such as those affected by conditions like rheumatic fever or infective endocarditis, can disrupt normal blood flow through the heart and contribute to the development of
Certain organisms like the Coxsackie B virus, Human Immunodeficiency virus (HIV), and Chagas disease are known to be associated with the development of cardiomyopathy.
Autoimmune diseases, such as rheumatoid arthritis or lupus, can cause inflammation and damage the heart muscle, leading to secondary
Illicit drug use, particularly cocaine and amphetamines, can cause damage to the heart muscle and increase the risk of cardiomyopathy.
The symptoms of cardiomyopathy can vary depending on the type and severity of the condition. Common symptoms include:
Various diagnostic tests can detect the presence of cardiomyopathy. Common diagnostic tests are discussed below:
EKG is a common diagnostic test used to assess the electrical activity of the heart and can provide valuable information for diagnosing cardiomyopathy. While an EKG alone cannot definitively diagnose cardiomyopathy, it can help detect abnormalities in heart rhythm and conduction, which may indicate underlying cardiac issues.
An echocardiogram is a noninvasive test that uses sound waves to create detailed images of the heart’s structure and function. It can help identify abnormalities in heart size, shape, and function and assess the heart’s pumping ability.
Blood tests help assess levels of certain enzymes and proteins that can indicate heart muscle damage. These may include cardiac troponin and brain natriuretic peptide (BNP).
MRI provides detailed images of the heart’s structure and can detect abnormalities in the heart muscle, valves, and blood It is particularly useful for evaluating myocardial tissue characteristics and detecting scar tissue.
CT scans can provide detailed images of the heart and blood vessels, helping to identify structural abnormalities, assess coronary artery disease, and evaluate heart function.
Genetic testing may be recommended in cases where a genetic component to cardiomyopathy is It helps to identify specific genetic mutations associated with the condition.
This procedure involves inserting a tube called a catheter into a blood vessel in the arm, groin, thigh, or neck, which is then guided to the heart. It helps to measure heart chamber pressures to assess for heart failure, obtain blood samples to evaluate oxygen levels and heart function and take an endomyocardial biopsy to diagnose specific types of cardiomyopathy or myocarditis.
Coronary angiography is a specialized X-ray imaging technique used to visualize the coronary arteries. It helps to rule out CAD as a cause of cardiomyopathy by detecting blockages or narrowing in the coronary It can also guide treatment decisions, such as angioplasty or bypass surgery if significant CAD is present.
It is a minimally invasive procedure and is sometimes utilized in diagnosing cardiomyopathy. It involves extracting a small tissue sample from the heart muscle. This biopsy aids in identifying specific types of cardiomyopathies or myocarditis, providing crucial insights for accurate diagnosis and treatment planning.
The treatment of cardiomyopathy aims to manage symptoms, improve heart function, prevent complications, and enhance overall quality of life.
Here is a list of five things you can do to help you with your cardiomyopathy.
Heart Failure Medications include angiotensin-converting enzyme inhibitors (Enalapril, Lisinopril), Angiotensin II Receptor Blockers (Losartan, valsartan), beta-blockers (carvedilol, metoprolol), and diuretics(spironolactone, Eplerenone). These medications are commonly prescribed to alleviate heart failure symptoms, enhance heart function, and decrease fluid retention.
Pacemakers are essential in managing certain types of cardiomyopathy, particularly those associated with rhythm Indicated primarily for patients with bradyarrhythmia like sinus node dysfunction or heart block, pacemakers work by monitoring the heart’s electrical activity and delivering electrical impulses to regulate heart rate and rhythm. Pacemaker implantation, a minimally invasive procedure performed under local anesthesia, involves inserting leads into the heart through veins and placing the pulse generator under the skin.
ICDs play a crucial role in managing cardiomyopathy, especially in cases with a risk of life-threatening ventricular These devices continuously monitor the heart rhythm and are designed to deliver a shock when they detect a dangerous arrhythmia such as ventricular tachycardia or ventricular fibrillation. By restoring normal heart rhythm through electrical therapy, ICDs can prevent sudden cardiac arrest and potentially save lives. The implantation procedure involves placing leads into the heart and positioning the device under the skin, typically in the chest area.
The LifeVest is a wearable cardioverter defibrillator (WCD) designed for patients at risk of sudden cardiac arrest who are not immediate candidates for an ICD or who require temporary protection after an ICD removal. It is a garment worn directly against the skin, typically over the torso, with electrodes integrated into the fabric. The LifeVest continuously monitors the patient’s heart rhythm, and if it detects a life-threatening arrhythmia, it delivers a shock to restore normal rhythm. Unlike permanent ICDs, the LifeVest is non-invasive and can be worn during daily activities, providing continuous protection without surgical implantation. This device serves as a bridge therapy, offering temporary protection while patients await further evaluation or as a transitional measure after ICD implantation or explantation.
CRT is a specialized treatment for certain types of cardiomyopathy, particularly those associated with heart failure and electrical It involves implanting a device similar to a pacemaker, called a CRT device, which delivers precisely timed electrical impulses to the heart’s ventricles. These impulses help synchronize the contractions of the heart’s chambers, improving its overall pumping efficiency. CRT is typically recommended for individuals with heart failure who have a widened QRS complex on their EKG, indicating electrical desynchrony.
Surgical interventions for cardiomyopathy aim to address specific underlying issues contributing to heart dysfunction and improve overall cardiac function.