Celiac Disease – Symptoms, Diagnosis, and Treatment

What is Celiac Disease?
Celiac disease is a common immune-mediated inflammatory illness of the small intestines. It is brought on by sensitivity to dietary gluten and similar proteins in those with genetic susceptibility. The condition is often termed “gluten-sensitive enteropathy” or “celiac sprue.” An autoimmune disease arises when the body’s own immune system attacks its tissues and organs.
Symptoms of Celiac Disease
Some people have celiac disease, which is silent, meaning they don’t exhibit any signs of the condition. However, individuals with silent gluten-sensitive enteropathy disease have immune proteins (antibodies) typical of celiac disease in their blood. We like to remember gluten-sensitive enteropathy disease with gastrointestinal and extraintestinal symptoms.
1. Gastrointestinal Symptoms
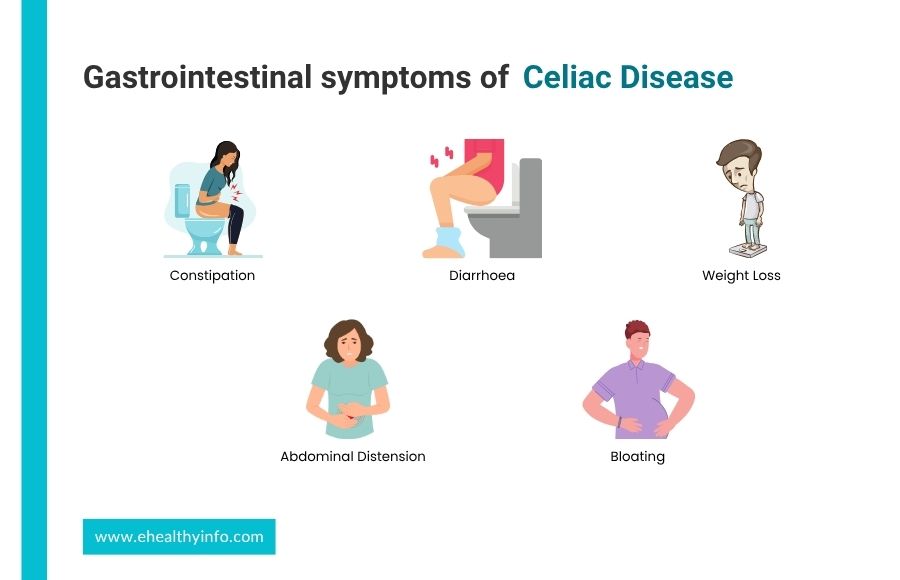
Some people have constipation or diarrhea that does not remit, an inability to absorb nutrients properly, weight loss, stomach discomfort, abdominal distension, or bloating. Diarrhea and poor nutrient absorption are symptoms of intestinal injury, which can induce weight loss.
2. Extraintestinal Symptoms

- Chronic mouth sore
- Loss of dental enamel
- Thinning of bones and premature osteoporosis
- Iron deficiency anemia
- Folate or vitamin B12 deficiency
- Dermatitis herpetiformis- a typical form of skin rash on the elbows and knees
- Fatigue
- Reduced fertility
- Abnormal tingling sensations on the extremities or reduced sensations with balance issues
Causes and Risk Factors for Celiac Disease
Celiac disease is brought on by an abnormal immune response brought on by gluten consumption. However, inflammation of the gastrointestinal system is the common cause of gluten-sensitive enteropathy disease. The following risk factors put a person at moderate to high risk for celiac disease:

- Relatives in the first and second degrees who have gluten-sensitive enteropathy disease: There is a 4–15% risk that parents, siblings, or children (first-degree relatives) of gluten-sensitive enteropathy disease patients will also have the condition. The inheritance pattern is uncertain, though.
- Diabetes mellitus type 1
- Thyroiditis and other autoimmune diseases
- Turner and Down syndromes
- Pulmonary hemosiderosis
How Will Your Doctor Diagnose Celiac Disease?
Many of the signs and symptoms of celiac disease are generic and can appear in various illnesses. Gluten-sensitive enteropathy disease frequently remains undiagnosed and untreated. Most persons who experience one or more of these unclear health issues do not have gluten-sensitive enteropathy disease. Accurate gluten-sensitive enteropathy disease diagnosis can often take 6 to 10 years following the onset of symptoms.
It is preferable to do all tests for gluten-sensitive enteropathy disease on patients when on a gluten-containing diet. Serologic testing needs to be done in individuals with no signs and symptoms of gluten-sensitive enteropathy disease. In individuals with a high likelihood of having celiac disease (those with signs and symptoms), serologic testing and small intestinal biopsies should be carried out, regardless of the results of the celiac-specific serology.

- Serologic evaluation: The single test for diagnosing adult gluten-sensitive enteropathy disease is the tissue transglutaminase (tTG)-IgA antibody. During the process, the total IgA levels are measured simultaneously. If someone has IgA deficiency, IgG-based testing using deamidated gliadin peptide (DGP)-IgG is carried out if someone has IgA deficiency.
- Endoscopy with small bowel biopsy: Upper GI endoscopy (a procedure where a small tube containing a camera is inserted into one’s alimentary tract via mouth) with a small intestinal biopsy is recommended to identify gluten-sensitive enteropathy disease in patients with positive serologic testing.
Adults with symptoms who refuse or are unable to have an upper GI endoscopy but who have high tissue transglutaminase IgA levels (>10-fold rise beyond the upper limit of normal) and a positive endomysial antibody (EMA) in a second blood sample can be identified as potential celiac disease patients.
Complications With Untreated Celiac Disease
Several different body organs and systems may have issues due to inflammation and inadequate nutrition absorption in afflicted individuals. These health issues could be:

- Iron deficiency anemia (low red blood cell count)
- Vitamin deficiencies
- Osteoporosis (low bone mineral density)
- Dermatitis herpetiformis (itchy skin rashes)
- Tooth enamel defects
- Chronic fatigue & joint pain
- Poor growth
- Delayed puberty
- Infertility or recurrent miscarriages
- Neurological issues such as migraine, depression, attention-deficit/hyperactivity disorder (ADHD), and repeated seizures (epilepsy)
You are at an increased risk of cancers of the intestines, such as small intestine or esophageal cancer, due to the chronic inflammation brought on by celiac disease.
Treatment for Celiac Disease
Dietary counseling is the first step in treating celiac disease patients. A lifetime commitment to a strict gluten-free diet is currently the only effective therapy for gluten-sensitive enteropathy disease. The management of celiac disease involves:

- A consultation with a qualified dietician
- Sensitization regarding the condition
- Maintaining a gluten-free diet for life
- Recognizing and addressing nutritional deficiencies
- Access to an advocacy organization
- Long-term, ongoing monitoring by a diverse team
- Patients should undergo testing for vitamin deficiencies (A, D, E, and B12), as well as for deficiencies in copper, zinc, carotene, folic acid, ferritin, iron, and prothrombin time (PT)
- DXA (dual-energy x-ray absorptiometry) scans should be used to assess patients for bone loss
- Hyposplenism (loss of splenic function) is related to celiac disease. Hence, it is advised to provide the pneumococcal vaccination as a preventative measure.
General Dietary Tips For all People With Celiac Disease
- Wheat, rye, and barley are the primary sources of dietary gluten and should be avoided.
- Rice, corn, buckwheat, and potatoes are all safe options.
- Carefully read the labels on prepared meals and condiments, paying close attention to any possible gluten-containing stabilizers or emulsifiers.
- Wine, vinegar, and distilled alcoholic drinks are gluten-free. However, as they are frequently manufactured from gluten-containing grains and are not distilled, beers, ales, lagers, and malt vinegar should be avoided.
- Patients whose symptoms seem aggravated by lactose-containing products should avoid them.
When to See Your Doctor?
You should see a doctor if you experience symptoms of celiac disease or have a family history of gluten-sensitive enteropathy disease, or have another autoimmune disorder; you may be at higher risk and should consider getting tested.
Questions For Your Doctor
- Are there any specific precautions people with celiac disease should take when eating out or traveling?
- How often should people with celiac disease be monitored?
- What should people with celiac disease do if they accidentally consume gluten?
- What are the long-term complications of celiac disease?
- Is it possible for celiac disease to be misdiagnosed or go undetected?
References
Return to Home
