Chronic kidney disease (CKD)
Chronic Kidney Disease: Everything You Need to Know?
What is Chronic Kidney Disease (CKD)?
Chronic kidney disease (CKD) is a progressive and potentially debilitating condition affecting millions worldwide. It is characterized by the gradual loss of kidney function over time, leading to a decline in the kidney’s ability to filter waste products and excess fluids from the blood. CKD can profoundly impact an individual’s overall health and quality of life, as it increases the risk of cardiovascular disease, complications related to fluid and electrolyte imbalances, and the need for dialysis or kidney transplantation. Understanding the causes, risk factors, symptoms, diagnosis, and management of CKD is crucial for early detection, intervention, and optimal care.
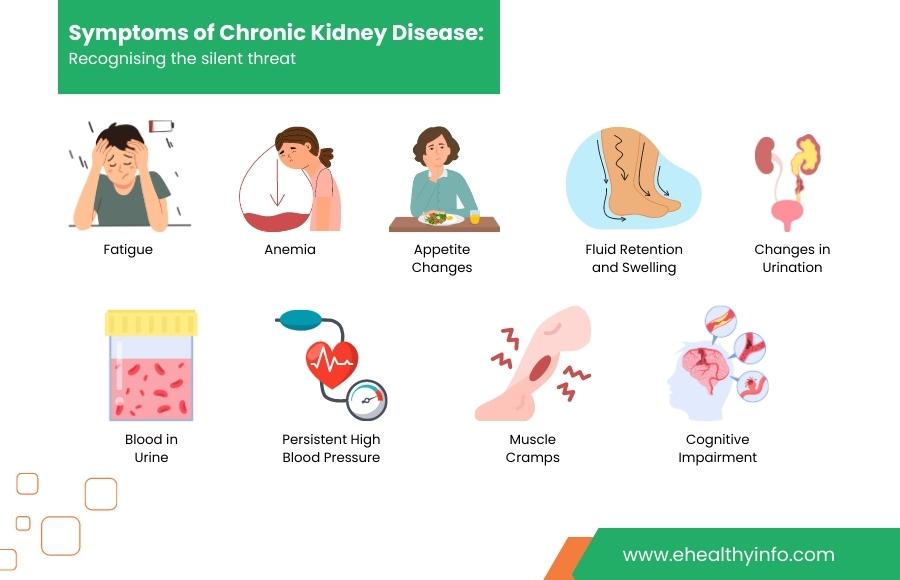
Symptoms Of Chronic Kidney Disease
Chronic kidney disease (CKD) often develops gradually and may be asymptomatic in its early stages. However, as the disease progresses, symptoms can manifest, indicating a decline in kidney function. Here are some common symptoms associated with chronic kidney disease:
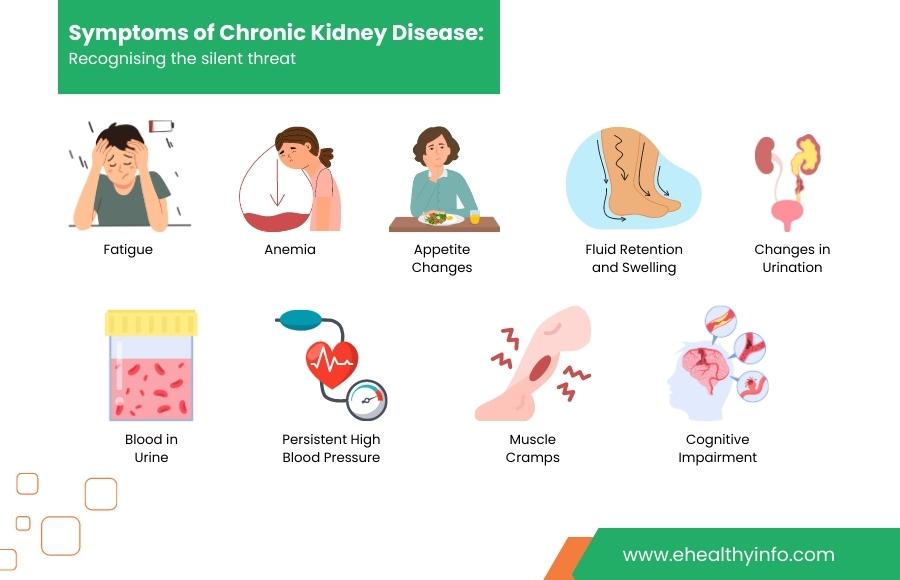
- Fatigue: Persistent fatigue and a general feeling of weakness or lack of energy can be early signs of CKD.
- Anemia: The kidneys play a crucial role in producing a hormone called erythropoietin, which stimulates red blood cell production. In CKD, reduced kidney function can lead to anemia, resulting in fatigue.
- Fluid Retention and Swelling: Impaired kidney function can cause fluid retention in the body, leading to swelling in the legs, ankles, feet, and face. This is known as edema due to the kidneys’ reduced ability to remove excess fluid and sodium from the bloodstream.
- Changes in Urination: CKD can cause changes in urination patterns depending on the stage of kidney damage. These may include:
-
- Increased frequency of urination, especially at night (nocturia).
- Decreased urine output or difficulty in urination.
- Foamy or bubbly urine, indicating the presence of excess protein (proteinuria).
- Blood in Urine: The presence of blood in the urine, known as hematuria, can be a sign of kidney damage. It may appear pink, red, or cola-colored.
- Persistent High Blood Pressure: The kidneys regulate blood pressure. Chronic kidney disease can lead to hypertension (high blood pressure), which, in turn, can further damage the kidneys, creating a vicious cycle.
- Appetite Changes: CKD can cause a loss of appetite, changes in taste, and nausea. As waste products build up in the blood, they can affect the digestive system, leading to GI upsets.
- Muscle Cramps and Restless Legs Syndrome: Electrolyte imbalances, such as low calcium and potassium levels, commonly occur in CKD. These imbalances can result in muscle cramps, especially in the legs, and a condition called restless legs syndrome, characterized by an uncontrollable urge to move the legs.
- Cognitive Impairment: In advanced stages of CKD, the accumulation of toxins in the blood can lead to cognitive changes, including difficulty concentrating, memory problems, and overall mental fogginess.
It’s important to note that the severity and presentation of symptoms can vary depending on the stage of CKD and individual factors. Not everyone with CKD will experience all of these symptoms.
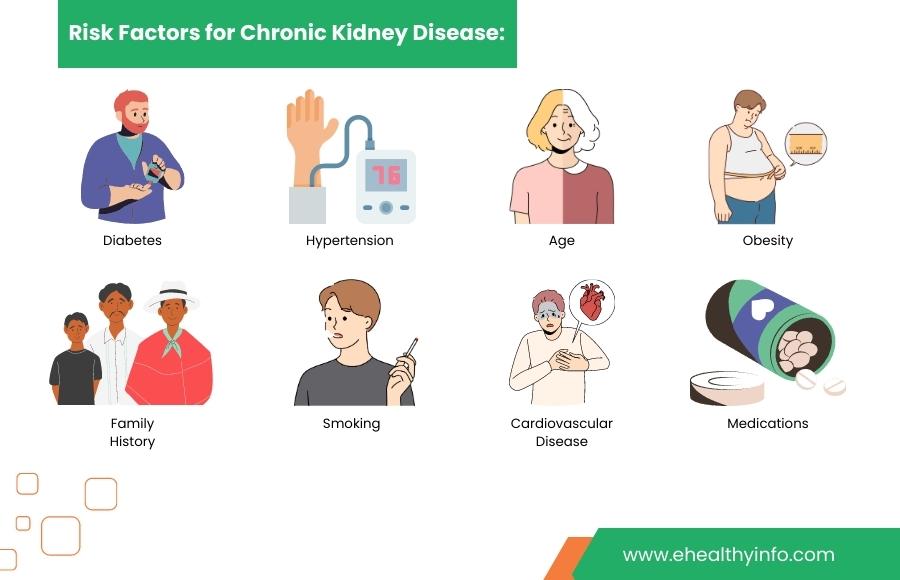
What Puts You At Risk Of CKD?
Chronic kidney disease is influenced by various risk factors. Recognizing these factors can help individuals identify their vulnerability and take proactive measures to protect their kidney health. Here are some common risk factors associated with the development of CKD:
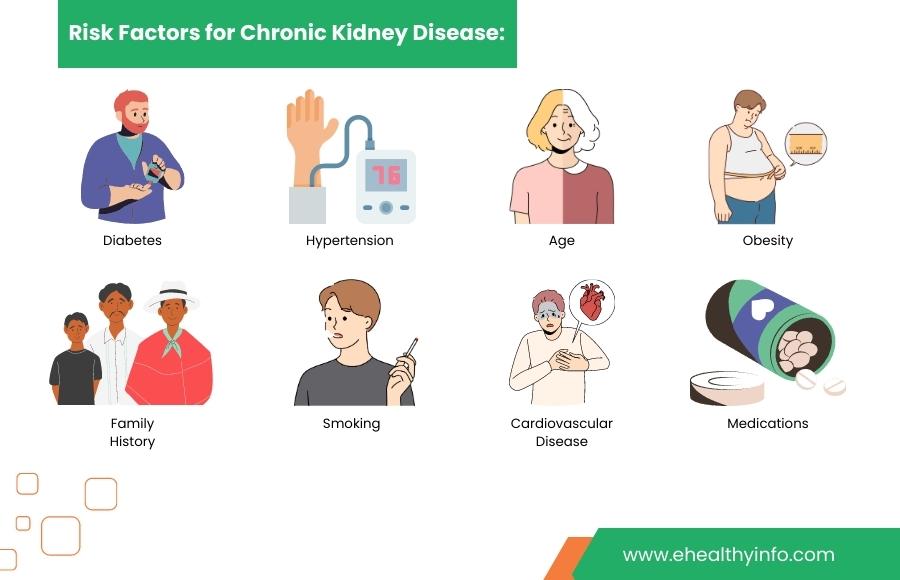
- Diabetes: Uncontrolled or poorly managed diabetes significantly increases the risk of developing CKD. High blood sugar levels can damage the blood vessels in the kidneys, impairing their ability to function properly.
- Hypertension (High Blood Pressure): Chronic high blood pressure strains the kidneys’ blood vessels, gradually causing damage over time. Hypertension is a leading cause of CKD and often coexists with other risk factors.
- Family History: A family history of kidney disease or a genetic predisposition to certain kidney conditions can increase the risk of developing CKD. Genetic factors can influence susceptibility to kidney damage and the progression of kidney disease.
- Age: The risk of CKD increases with age. Older individuals are more prone to developing kidney damage and impaired kidney function due to the cumulative effects of other risk factors and natural aging processes.
- Obesity: Excess body weight, particularly when accompanied by unhealthy lifestyle habits, can contribute to the development of CKD. Obesity is linked to conditions such as diabetes and hypertension, major kidney disease risk factors.
- Smoking: Smoking harms blood vessels, including those in the kidneys. It can accelerate the progression of kidney damage and worsen existing kidney conditions.
- Cardiovascular Disease: Conditions such as heart disease, stroke, and peripheral artery disease can increase the risk of CKD. The heart and kidneys are closely connected, and any dysfunction in the cardiovascular system can impact kidney health.
- Other Medical Conditions: Certain medical conditions, such as autoimmune diseases, chronic urinary tract infections, and kidney abnormalities present from birth, can predispose individuals to CKD.
- Medications and Toxins: Prolonged use of certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and some antibiotics, as well as exposure to certain toxins, can contribute to kidney damage and increase the risk of CKD.
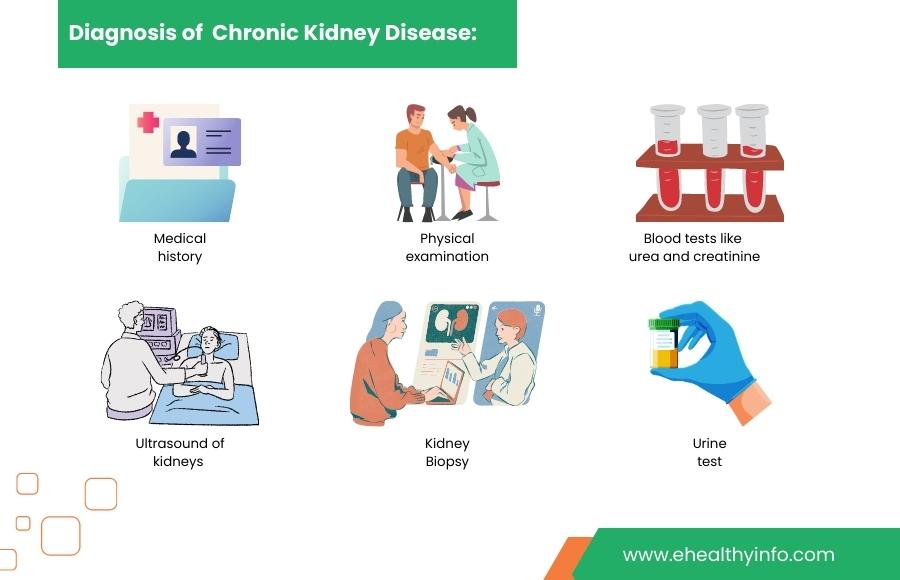
How is Chronic Kidney Disease Diagnosed?
Diagnosing chronic kidney disease involves a comprehensive evaluation that combines medical history, physical examination, laboratory tests, and imaging studies. The diagnostic process aims to assess kidney function, determine the stage of CKD, identify the underlying cause, and monitor any associated complications. Here are the key components of diagnosing CKD:
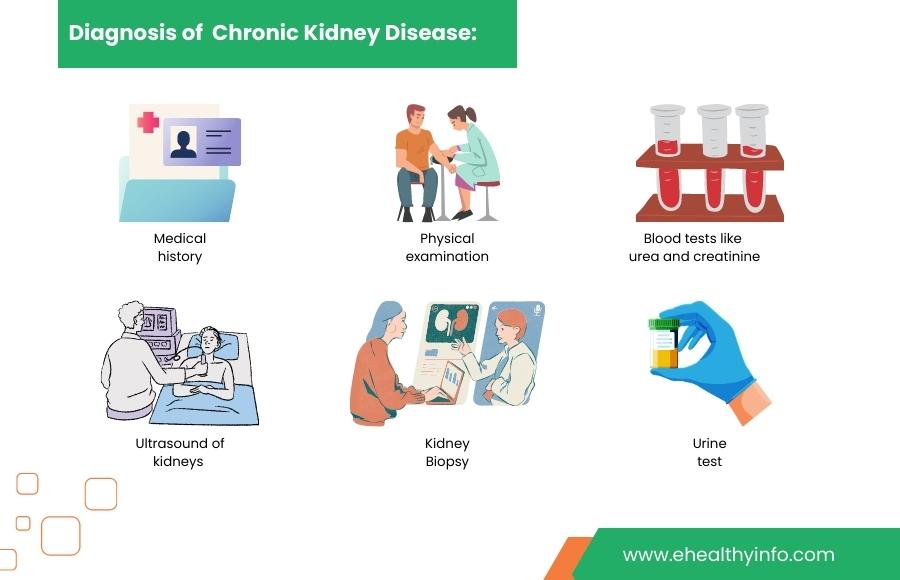
1. Medical History and Physical Examination: The healthcare provider will review your medical history, including any known risk factors or symptoms. A physical examination may be conducted to check for signs of fluid retention, hypertension, or other indicators of kidney damage.
2. Blood Tests: Blood tests are crucial in assessing kidney function and determining the presence of CKD. The following blood tests are commonly performed:
- Serum Creatinine: Elevated creatinine levels, a waste product in the blood, indicate impaired kidney function.
- Blood Urea Nitrogen (BUN): BUN levels are measured to assess the efficiency of kidney filtration.
- Estimated Glomerular Filtration Rate (eGFR): This calculation estimates the kidney’s ability to filter waste products from the blood. A low eGFR indicates reduced kidney function.
3. Urine Tests: Urine tests help evaluate kidney function and detect the presence of abnormalities such as proteinuria (excess protein in the urine) or hematuria (blood in the urine). A 24-hour urine collection may be requested to quantify the protein excreted.
4. Imaging Studies: Imaging techniques such as a renal ultrasound, CT scan, or MRI may be utilized to assess the structure and size of the kidneys. These tests can help identify any abnormalities, blockages, or kidney stones that may contribute to CKD.
5. Kidney Biopsy (in some cases): In certain situations, a kidney biopsy may be recommended to obtain a small sample of kidney tissue for microscopic examination. This procedure helps identify the underlying cause of CKD and provides valuable insights for appropriate management.
⇒ Once CKD is diagnosed, your healthcare provider determines the stage of the disease based on the eGFR. The staging system helps guide treatment decisions and determine the appropriate management plan.
Complications Of Chronic Kidney Disease
CKD is a multifaceted condition that can give rise to various complications, affecting the kidneys and numerous other organs and systems within the body. Here are some common complications associated with chronic kidney disease:
- Cardiovascular Disease: Individuals with CKD are more likely to develop cardiovascular diseases such as heart attacks, heart failure, and stroke. The kidneys and cardiovascular system are closely interconnected, and the impaired kidney function in CKD can lead to an imbalance in fluid volume, electrolytes, and hormones, contributing to cardiovascular complications.
- High Blood Pressure (Hypertension): Chronic kidney disease can cause or exacerbate hypertension. Elevated blood pressure can further damage the kidneys, creating a vicious cycle. Proper blood pressure management is vital in slowing the progression of CKD and reducing the risk of cardiovascular events.
- Anemia: CKD often leads to anemia, characterized by decreased red blood cell count and a reduced ability to carry oxygen throughout the body. Anemia can cause fatigue, weakness, shortness of breath, and other symptoms, affecting overall well-being and quality of life.
- Bone and Mineral Disorders: Impaired kidney function can disrupt the balance of minerals in the body, leading to bone disorders such as osteoporosis and osteomalacia. CKD can result in abnormal calcium and phosphorus levels, weakened bones, and an increased risk of fractures.
- Fluid and Electrolyte Imbalances: The kidneys play a crucial role in maintaining fluid and electrolyte balance in the body. In CKD, these regulatory functions are impaired, leading to fluid retention, sodium and potassium imbalances, and complications such as edema, hypertension, and irregular heartbeat.
- Acidosis: CKD can cause metabolic acidosis, a condition characterized by an imbalance in the body’s acid-base equilibrium. The kidneys are responsible for eliminating excess acid from the bloodstream, and their dysfunction in CKD can lead to an accumulation of acid, affecting various body systems and potentially causing fatigue, confusion, and other symptoms.
- Impaired Immune Function: CKD weakens the immune system, making individuals more susceptible to infections, including urinary tract infections, respiratory infections, and skin infections. The body’s ability to fight infections is compromised, leading to more frequent and severe illnesses.
- End-Stage Renal Disease (ESRD): In advanced stages of CKD, when kidney function is severely impaired, end-stage renal disease may occur. Individuals may require dialysis or kidney transplantation to sustain life at this stage.
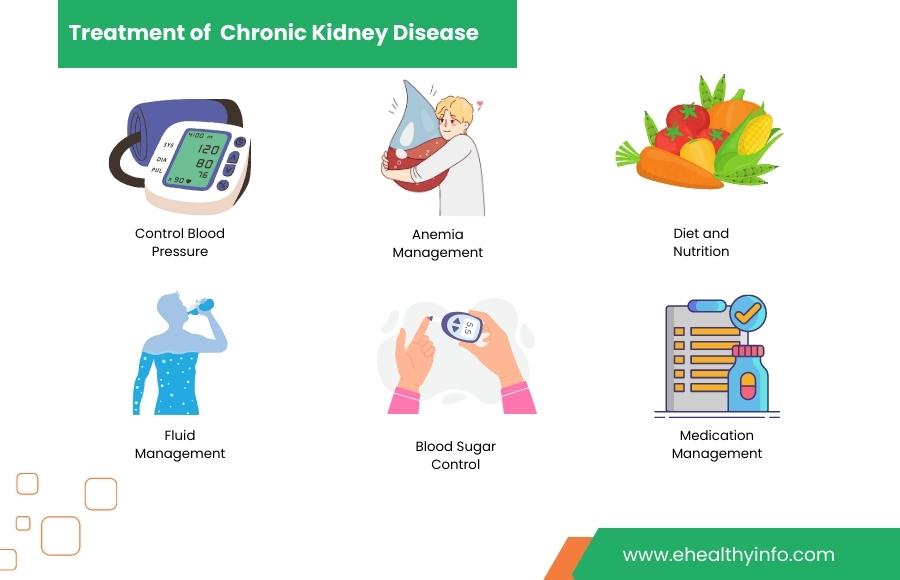
Treatment Of Chronic Kidney Disease
The treatment of chronic kidney disease (CKD) aims to slow the progression of the disease, manage symptoms, and prevent complications. Here are key treatment strategies commonly employed in CKD management:
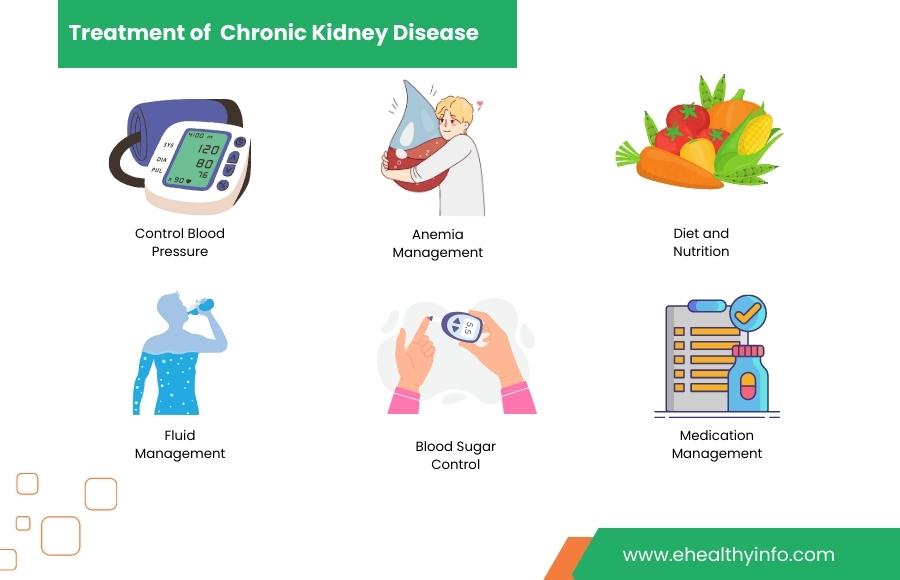
- Blood Pressure Control: Controlling high blood pressure is crucial in slowing the progression of CKD. Lifestyle modifications such as following a low-sodium diet, engaging in regular physical activity, and maintaining a healthy weight can help. Medications, such as angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARBs), may be prescribed to manage blood pressure effectively.
- Blood Sugar Control: For individuals with diabetes and CKD, proper management of blood sugar levels is essential. This may involve regularly monitoring blood glucose levels, adhering to a diabetic diet plan, taking prescribed medications or insulin, and maintaining a healthy lifestyle.
- Medication Management: Medications may be prescribed to address specific complications or underlying causes of CKD. These may include medications to manage high cholesterol levels, treat anemia, or address bone disorders. Adherence to prescribed medications and regular follow-up with healthcare professionals is important.
- Diet and Nutrition: A kidney-friendly diet is crucial in managing CKD. This may involve limiting sodium, phosphorus, and potassium intake, monitoring protein consumption, and making dietary adjustments based on individual needs. A registered dietitian experienced in kidney disease can provide personalized guidance and meal planning.
- Fluid Management: In advanced stages of CKD, fluid intake may need to be monitored and limited to prevent fluid retention. This helps maintain fluid balance and avoid complications associated with excess fluid buildup. Healthcare professionals provide recommendations based on individual needs.
- Anemia Management: Anemia is common in CKD due to reduced production of red blood cells. Medications such as erythropoiesis-stimulating agents (ESA) may be prescribed to stimulate red blood cell production. Iron supplements or intravenous iron therapy may also be recommended to address iron deficiency.
- Dialysis: In end-stage renal disease (ESRD), dialysis may be necessary to replace kidney function. There are two primary types of dialysis: hemodialysis, where blood is filtered through a machine, and peritoneal dialysis, where a dialysis solution is introduced into the abdomen to remove waste products. Dialysis helps maintain fluid and electrolyte balance and removes toxins from the body.
- Kidney Transplantation: Kidney transplantation may be considered for suitable candidates with ESRD. It involves replacing a failed kidney with a healthy donor kidney. Transplantation offers the potential for improved quality of life and a long-term solution to kidney failure.
Dialysis - Explained In A Minute
Dialysis plays a crucial role in individuals with end-stage renal disease (ESRD), where kidney function is significantly impaired. Dialysis is a life-sustaining treatment by performing the vital functions the kidneys can no longer adequately fulfill.
There are two primary types of dialysis: Hemodialysis and Peritoneal dialysis
Hemodialysis involves using a dialysis machine that filters the blood outside the body, while peritoneal dialysis utilizes the body’s peritoneal membrane as a natural filter. Both methods help remove waste products, excess fluids, and toxins from the body. Dialysis sessions are typically scheduled several times a week, and adherence to the treatment plan is vital for maintaining fluid balance, electrolyte levels, and overall well-being. Although dialysis is a significant commitment and may involve lifestyle and dietary restrictions adjustments, it offers a lifeline for individuals with CKD, allowing them to manage their condition, alleviate symptoms, and improve their quality of life.
Dialysis may also serve as a bridge to kidney transplantation for eligible candidates, offering the potential for a long-term solution to kidney failure. Regular communication and collaboration with healthcare professionals are essential for optimal dialysis outcomes and effective management of CKD.
Tips To Prevent Chronic Kidney Disease
CKD is a progressive condition; however, there are measures individuals can take to reduce the risk of developing CKD or delay its progression. Here are key strategies for preventing CKD:
- Undergo regular health check-ups and screenings to monitor blood pressure, blood sugar levels, and kidney function.
- Manage existing health conditions effectively, such as diabetes, high blood pressure, and cardiovascular diseases.
- Maintain healthy blood pressure through lifestyle modifications and medication adherence.
- Control blood sugar levels for individuals with diabetes through medication, diet, and regular monitoring.
- Minimize exposure to nephrotoxic substances, including certain medications and recreational drugs.
- Avoid illicit drug use and be cautious with medication and supplement usage.
- Adopt a healthy lifestyle with regular physical activity, weight management, and limited alcohol consumption.
When To See Your Doctor?
It is important to see your doctor for chronic kidney disease (CKD) at various stages and under different circumstances. Here are situations when you should consider seeking medical attention:
- Diagnosis and Monitoring: Seek medical attention if you suspect CKD or have risk factors. Regular monitoring is necessary for diagnosed CKD.
- Worsening Symptoms: Consult your doctor for evaluation if symptoms worsen, such as fatigue, appetite changes, swelling, uncontrolled blood pressure, or fluid balance difficulties.
- Medication Management: Regularly follow up with your doctor to monitor medication effectiveness, adjust dosages, and discuss any concerns or side effects.
- Changes in Lab Results: Seek medical attention if there are significant changes in blood test results, such as increased creatinine levels or decreased eGFR.
- Complications or New Symptoms: Promptly seek medical attention for new symptoms or complications related to CKD, such as high blood pressure, anemia, bone disorders, or electrolyte imbalances.
- Preparation for Dialysis or Transplant: If advanced CKD requires dialysis or transplantation, your doctor will guide you and discuss treatment options.
- Emotional and Psychosocial Support: Discuss emotional well-being concerns with your doctor, who can provide support or refer you to a mental health professional if needed.
Questions To Ask Your Doctor
- What stage of CKD am I currently in, and what does it mean for my kidney function?
- What is the underlying cause of my CKD?
- What lifestyle changes should I make to help slow the progression of CKD?
- Are there any specific dietary restrictions or recommendations I should follow?
- What medications are prescribed to manage my CKD, and what are their potential side effects?
- How often should I have my kidney function monitored through blood tests and check-ups?
- Are there any additional tests or screenings I should undergo to monitor my overall health and the progression of CKD?
- Should I see a nephrologist to manage my CKD?
- Are there any new treatment options or clinical trials available that may benefit me?
- How can I effectively manage associated complications, such as high blood pressure, anemia, or bone disorders?
- What are the warning signs of worsening kidney function or potential complications should I be aware of?
- Are there any lifestyle modifications or precautions I should consider when traveling or during specific activities?
- Can a support group or resources help me navigate living with CKD?