Crohn’s Disease – Symptoms, Causes, Diagnosis and Treatment

| Highlights of Crohn’s Disease
- Crohn’s disease is an inflammatory bowel disease that can affect any part of the digestive tract, with the small intestine and colon being the most commonly affected areas.
- Crohn’s disease persists throughout life and follows a pattern of relapses and periods of improvement.
- While the exact cause of inflammatory bowel disease remains unclear, evidence suggests it stems from an abnormal immune response in the gut triggered by environmental factors like drugs, toxins, infections, or gut microbes in individuals with certain genetic susceptibilities.
- Smokers have a higher risk of developing Crohn’s disease than nonsmokers.
- To better manage Crohn’s disease, try increasing fluid intake, eating smaller, more frequent meals, and maintaining a food diary to identify possible triggers.
What is Crohn’s Disease?
Crohn’s disease is one component of inflammatory bowel disease (IBD), which is characterized by immune system-driven inflammation in the gastrointestinal tract. In Crohn’s disease, the inflammation affects the entire bowel wall, from the inner mucosa to the outer serosa layer. This inflammation in various parts of the bowel and the systemic impact of the disease lead to a range of clinical presentations and long-term risks.
In the US, 721 out of every 100,000 people are living with IBD, which includes both Crohn’s disease and Ulcerative Colitis. [1]
Causes and Risk Factors of Crohn’s Disease
The exact cause of Crohn’s disease remains uncertain, but here are some factors that might be involved:
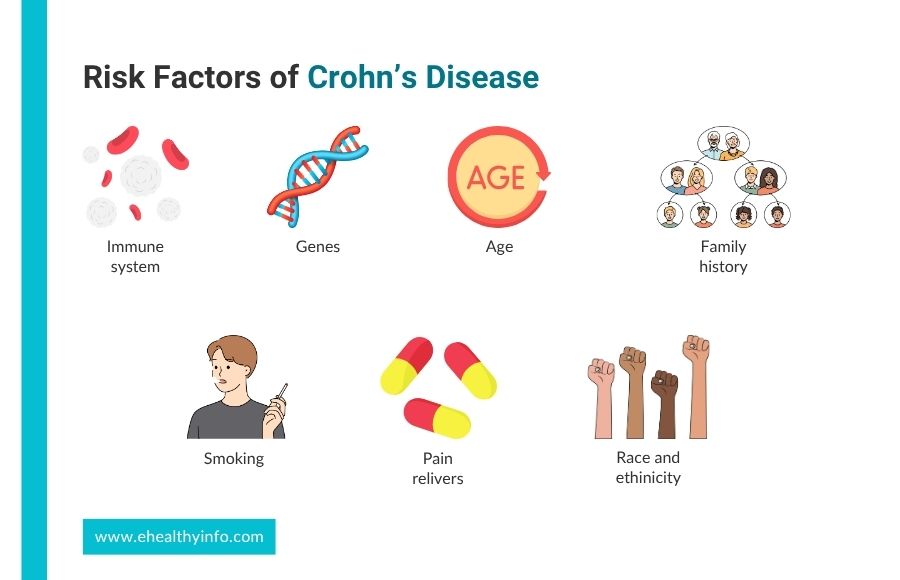
1. Immune system
Your immune system might mistakenly attack healthy cells when certain gut bacteria trigger a response, causing inflammation. This imbalance in gut bacteria weakens the gut’s immune system. [2]
2. Genes
Crohn’s disease sometimes runs in families, so if you have a close relative with it, you might be more likely to get it, too.
3. Age
Crohn’s disease can affect people of any age. It is, however, most commonly diagnosed in young adults. Most cases are identified in individuals between the ages of 15 and 35.
4. Family history
If one of your parents has Crohn’s disease, your chances of developing it are around 7 to 10 percent. However, if both of your parents have the condition, your risk increases significantly to about 35 percent. [3]
5. Race and Ethnicity
Ashkenazi Jews are about four times more likely to get Crohn’s disease compared to non-Jews in the same area. While most people with IBD worldwide are not Jewish, the Jewish community is significantly more affected by these conditions. [4]
6. Other factors
Certain things like smoking, taking certain pain relievers like aspirin or ibuprofen, antibiotics, and birth control pills might slightly increase your chances of getting Crohn’s disease. A diet high in fat could play a role in Chron’s disease. [5]
Symptoms of Crohn’s Disease
Patients often go through a cycle of active symptoms, known as flares, followed by remission, when symptoms lessen or disappear. These fluctuating symptoms can go on from weeks to years and range from mild to severe. The five most common symptoms are:

1. Chronic Diarrhea
During an IBD flare, the intestine lining swells up, making it hard to absorb all the liquid. This can lead to loose, watery, or even completely liquid stools. This is sometimes accompanied by the urgency to pass stool when the bowels are empty. Sometimes, you might also notice blood, mucus, pus, and loose stool.
2. Abdominal pain
Pain and cramping are frequent symptoms of Crohn’s disease. Many patients feel abdominal pain on the lower right side or around their navel, usually about 1 to 2 hours after eating. The pain tends to worsen during a flare-up. While pain in the small intestine is common, cramps can occur regardless of which part of the intestine is affected.
3. Weight loss
Inflammation makes it harder to absorb nutrients, leaving you malnourished. Furthermore, dehydration and a reduced appetite caused by diarrhea and cramps may prevent the body from getting enough energy and essential nutrients it needs and cause unintentional weight loss.
4. Fatigue
Fatigue is a common experience for people with Crohn’s and Colitis, affecting around 72% of individuals during a flare-up and about 30% during remission. In a study, individuals described their fatigue as “brain fog,” feeling completely wiped out, or being “very, very weary.” This fatigue doesn’t improve with rest. [6]
5. Blood in stool
Some people with Crohn’s disease might not have any bleeding. Unlike ulcerative colitis, bleeding is less common in Crohn’s. But if the lower colon and rectum are affected, you might see blood in your stool during flare-ups. [7]
Diagnosis of Crohn’s Disease
No single test exists to diagnose Crohn’s disease. There are a variety of tests to confirm the diagnosis of Crohn’s disease, which may include:

1. Lab Tests
- Blood tests: Different blood tests are performed to diagnose Chron’s disease. A complete blood cell count can show changes in your red and white blood cells. Fewer or smaller red blood cells may indicate anemia, while a higher white blood cell count could mean inflammation or infection. Specific antibodies like Perinuclear Anti-Neutrophil Cytoplasmic Antibodies (pANCA), Anti-Saccharomyces Cerevisiae Antibodies (ASCA), and Outer Membrane Porin C (Omp C) can help diagnose Crohn’s disease. [8]
- Stool test: When you take a stool test, your doctor will give you a container to collect a stool sample. They will tell you where to send or take the kit for analysis. A stool test helps rule out other causes of digestive diseases, including tests like fecal calprotectin, which detect inflammation in the intestines. It helps distinguish between IBD and Irritable Bowel Syndrome.
2. Intestinal Endoscopy
Intestinal endoscopy is the best way to diagnose Crohn’s disease and check for other issues. It shows how your digestive tract looks and checks for any fissures, ulcers, or changes caused by inflammation. [9]
- Colonoscopy: This procedure uses a thin tube with a camera to visualize the rectum and colon. If Crohn’s disease is suspected, biopsies or tissue samples might be taken.
- Upper GI endoscopy: During an upper GI endoscopy, a doctor guides the endoscope down your throat to see inside your stomach and duodenum.
- Enteroscopy: Your small intestine is checked using a longer scope, which might involve different techniques, such as push enteroscopy or capsule endoscopy.
3. Upper GI Series
An upper GI series involves your doctor using X-rays, fluoroscopy, and a chalky liquid called barium to examine your upper digestive system.
4. Computed Tomography (CT) Scan
This imaging mode helps to see a super detailed picture of your insides, including your digestive tract. CT scans help determine if you have Crohn’s disease and spot any problems it might be causing in your body, like inflammation, abnormal connections (fistula), or narrowing (strictures) in your intestines.
5. Magnetic Resonance Imaging (MRI) Scan
An MRI scanner obtains a detailed picture of your organs and tissues using the help of a magnetic field and radio waves. Doctors use MRI to check for fistulas near your anus (called pelvic MRI) or in your small intestine (MR enterography). They may also use MRI to monitor Crohn’s disease without exposing younger people to radiation. [10]
Treatment of Crohn’s Disease
Currently, there is no cure for this disease, and treatments aren’t one-size-fits-all, either. The goals of treatment are to lessen inflammation, prevent symptoms from worsening, and keep the disease under control. Crohn’s disease can be controlled with medications, periods of bowel rest, and, in some cases, surgery.

1. Medications
Lots of people with Crohn’s disease require medication. The specific medications you need depend on your symptoms.
- Aminosalicylates: Aminosalicylates contain 5-aminosalicylic acid (5-ASA), which helps manage inflammation. They’re often prescribed for people with newly diagnosed Crohn’s disease and with mild symptoms, though contradictory findings have been shown regarding its efficacy in remission. [11] Examples include balsalazide, mesalamine, olsalazine, and sulfasalazine. When you’re under this medication, you might experience side effects such as diarrhea, headaches, heartburn, nausea, vomiting, and abdominal pain.
- Corticosteroids: Corticosteroids provide quick relief from inflammation and symptoms. However, long-term use is not advisable because of potential side effects like acne, bone loss, high blood glucose, high blood pressure, increased infection risk, mood swings, and weight gain. Examples include budesonide, hydrocortisone, methylprednisolone, and prednisone. [12]
- Immunomodulators: Immunomodulators reduce the activity of your immune system, which decreases inflammation in your digestive tract. Immunomodulators, such as 6-mercaptopurine (6-MP), azathioprine, cyclosporine, and methotrexate, help you go into remission or if you don’t respond to other treatments. However, they may have side effects such as low white blood cell count, fatigue, nausea, vomiting, and pancreatitis. [13]
- Biologic therapies: Biologic therapies target proteins your immune system produces to reduce inflammation in the intestines and achieve remission, especially if other medications haven’t been effective. Examples include anti-tumor necrosis factor-alpha therapies like adalimumab, certolizumab, and infliximab, as well as anti-integrin therapies like natalizumab and vedolizumab and anti-interleukin-12 and interleukin-23 therapy such as ustekinumab. However, one might have a toxic reaction to the medication and an increased risk of infections, particularly tuberculosis. [13]
- Other medications: Doctors may prescribe acetaminophen for mild pain relief, antibiotics for infection-related complications like abscesses and fistulas, and loperamide to alleviate severe diarrhea, though its use is usually short-term due to the risk of megacolon. Metronidazole doesn’t work in Crohn’s disease. [14]
2. Bowel Rest
If your disease is bad, your doctor might suggest resting your bowel. This means you’ll only drink certain liquids or nothing for a few days or weeks. During this time, your doctor might have you drink a special liquid with nutrients or give you nutrients through a tube in your stomach or vein. You might need to stay in the hospital, but sometimes you can do this at home. Most people’s intestines get better during bowel rest.
3. Surgery
Even with medications, many people with Crohn’s disease end up needing surgery. A study found that almost 60 percent of people had surgery within 20 years of being diagnosed. While surgery won’t cure Crohn’s disease, it can help with complications and improve symptoms. Doctors often suggest surgery for conditions like fistulas, life-threatening bleeding, intestinal blockages, and when medicines aren’t working well enough. [15]
- Small bowel resection: Small bowel resection is a surgical procedure where part of the small intestine is removed. It is often necessary for severe forms of disease, and it can be done either laparoscopically with small incisions and a camera or through open surgery with a larger incision.
- Subtotal colectomy: A subtotal colectomy, also known as a large bowel resection, is a procedure that removes a piece of the large intestine to treat severe Crohn’s disease. This procedure can be done with either laparoscopic colectomy, which uses small incisions and a camera, or open surgery, which uses a single bigger incision.
- Proctocolectomy and ileostomy: Proctocolectomy takes out your colon and rectum, while ileostomy creates a small opening in your belly called a stoma, usually from part of your ileum. The ostomy pouch, connected to the stoma, gathers stool outside the body. Since the stoma doesn’t have muscle control, stool passes through the stoma whenever it happens instead of the anus. If you have this surgery, you’ll have the ileostomy for life.
Complications of Crohn’s Disease
Crohn’s disease is a systemic condition with various complications affecting the intestines and other parts of the body. Some complications associated with Crohn’s disease include:

- Strictures in the intestines
- Formation of fistulas and abscesses
- Increased risk of colorectal carcinoma
- Ankylosing spondylitis, causing joint pain
- Eye conditions like episcleritis and iritis cause eye redness or blurry vision
- Skin changes such as erythema nodosum and pyoderma gangrenosum
- Anemia due to chronic inflammation
- Weakening of bones leads to osteoporosis [16]
Living with Crohn’s Disease
If you have Crohn’s disease, it’s important to take care of yourself to feel your best. Here are some things you can do:
1. Daily physical activity
Even a short walk, can help you feel better and reduce stress linked with Crohn’s disease.
2. Quit smoking
If you smoke, stopping can help you manage your Crohn’s better and reduce the chances of complications.
3. Stress management
Stress management techniques, such as mindfulness and relaxation exercises, are important to prevent symptom flare-ups. Social and emotional support from family, friends, and support groups can provide significant relief and encouragement.
Nutrition in Crohn’s Disease
Nutrition plays a crucial role in managing Crohn’s disease, as it can help reduce symptoms and promote overall health. Individuals with Crohn’s disease often experience difficulty absorbing nutrients due to inflammation in the digestive tract, making it essential to focus on a nutrient-dense diet. This includes eating foods like fruits, vegetables, lean proteins, and whole grains while avoiding foods that can trigger flare-ups, such as high-fat, high-fiber, or spicy foods. Small, frequent meals and adequate hydration are recommended to ease digestion and maintain energy levels. Keeping a food diary can help you identify and eliminate specific dietary triggers. Supplements may be necessary to address deficiencies in vitamins and minerals such as vitamin D, calcium, iron, and B12. [17]
Questions To Ask Your Doctor
- Is there a possibility that my child will develop Crohn’s disease?
- Will I require lifelong therapy?
- Can preventive measures help in preventing Crohn’s disease?
- How could being diagnosed with IBD impact my ability to conceive?
- Will Crohn’s disease affect my lifespan?
References
- Lewis JD, Parlett LE, Jonsson-Funk M, Brensinger CM, Pate V, Wu Q, et al. Incidence, Prevalence and Racial and Ethnic Distribution of Inflammatory Bowel Disease in the United States. Gastroenterology. 2023 Jul 1;165(5).
- Brown K, DeCoffe D, Molcan E, et al. Diet-induced dysbiosis of the intestinal microbiota and the effects on immunity and disease. Nutrients. 2012;4(8):1095–119.
- Crohn’s Disease [Internet]. American College of Gastroenterology. Available from: https://gi.org/topics/crohns-disease/
- Borren NZ, Conway G, Garber JJ, Khalili H, Budree S, Mallick H, et al. Differences in Clinical Course, Genetics, and the Microbiome Between Familial and Sporadic Inflammatory Bowel Diseases. J Crohns Colitis 2018;12(5):525–31.
- Ko Y, Butcher R, Leong RW. Epidemiological studies of migration and environmental risk factors in the inflammatory bowel diseases. World J Gastroenterol. 2014 Feb 7;20(5):1238-47. doi: 10.3748/wjg.v20.i5.1238. PMID: 24574798; PMCID: PMC3921506.
- Włodarczyk M, Makaro A, Prusisz M, Włodarczyk J, Nowocień M, Maryńczak K, et al. The Role of Chronic Fatigue in Patients with Crohn’s Disease. Life 2023;13(8):1692.
- Matsuoka K, Kobayashi T, Ueno F, Matsui T, Hirai F, Inoue N, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease. J Gastroenterol 2018;53(3):305–53.
- Mitsuyama K. Antibody markers in the diagnosis of inflammatory bowel disease. World J Gastroenterol 2016;22(3):1304.
- Spiceland CM, Lodhia N. Endoscopy in inflammatory bowel disease: Role in diagnosis, management, and treatment. World J Gastroenterol 2018;24(35):4014–20.
- Ahmad R, Ajlan AM, Eskander AA, Alhazmi TA, Khashoggi K, Wazzan MA, et al. Magnetic resonance imaging in the management of Crohn’s disease: a systematic review and meta-analysis. Insights Imaging 2021;12(1):118.
- Honap S, Sharma E, Samaan MA. 5-ASAs in Crohn’s Disease: Time to Stop the Salicylate? Dig Dis Sci 2022;67(7):2699–700.
- Farraj KL, Pellegrini JR, Munshi RF, Russe‐Russe J, Kaliounji A, Tiwana MS, et al. Chronic steroid use: An overlooked impact on patients with inflammatory bowel disease. JGH Open 2022;6(12):910–4.
- Rodríguez-Lago I, Gisbert JP. The Role of Immunomodulators and Biologics in the Medical Management of Stricturing Crohn’s Disease. J Crohns Colitis 2020;14(4):557–66.
- Bernstein CN, Eliakim A, Fedail S, Fried M, Gearry R, Goh KL, et al. World Gastroenterology Organisation Global Guidelines Inflammatory Bowel Disease. Journal of Clinical Gastroenterology. 2016;50(10):803–18.
- Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sandborn WJ, Loftus EV. Surgery in a population-based cohort of Crohn’s disease from Olmsted County, Minnesota (1970-2004). The American journal of gastroenterology [Internet]. 2012 [cited 2019 Dec 10];107(11):1693–701. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22945286
- Ranasinghe IR, Hsu R. Crohn Disease [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436021/
- Caio G, Lungaro L, Caputo F, Zoli E, Giancola F, Chiarioni G, et al. Nutritional Treatment in Crohn’s Disease. Nutrients 2021;13(5):1628.
Return to Home
