Epilepsy Demystified – Symptoms, Seizures, Treatment Options, and Types

Key Highlights
- Epilepsy is a chronic neurological disorder with recurrent seizures and is caused by abnormal electrical activity in the brain.
- Seizures can manifest in different ways, including focal seizures that originate in one area of the brain and generalized seizures that involve widespread electrical disturbances.
- Diagnosis of epilepsy involves a thorough evaluation of medical history, symptoms, and diagnostic tests like EEG and neuroimaging.
- Treatment typically includes antiepileptic medications, lifestyle modifications, and sometimes surgical interventions to control seizures and improve quality of life.
- Your doctor will gradually reduce the dosage and consider stopping your seizure medications entirely only after you have been seizure-free for a period of 2 to 4 years.
What is Epilepsy?
Epilepsy is a neurological disorder characterized by recurrent seizures. Seizures occur due to abnormal electrical activity in the brain and can lead to various symptoms, including convulsions, loss of consciousness, unusual sensations, or temporary confusion.
Epilepsy impacts individuals across all age groups, affecting approximately 50 million people worldwide and around 3.4 million individuals in the United States alone. The number of cases of epilepsy is leading to over one hundred thousand new diagnoses annually in the US, reflecting a rising trend in the condition’s incidence.
Types of Epilepsy
When we hear the word seizure, we think of muscle spasms, involuntary body movements, and a loss of consciousness. However, most seizures are surprisingly subtle and may be hard to recognize.
1. Generalized epilepsy
If a large part of the brain or the entire brain is involved, you may experience a loss of awareness without any warning. Your whole body may also stiffen or shake involuntarily. Generalized seizures are classified into different subtypes:
- Absence Seizures (petit mal seizures): During these seizures, you may have brief lapses of consciousness characterized by staring blankly or subtle movements such as eye blinking or lip-smacking.
- Tonic-Clonic Seizures (grand mal seizures): These are dramatic seizures presenting with loss of consciousness and stiffening of muscles (tonic phase), followed by rhythmic jerking movements (clonic phase).
- Myoclonic Seizures: You may have sudden, brief jerks or twitches of the muscles, often involving the arms and legs.
- Clonic Seizures: This is the type of epilepsy where you will have repetitive, rhythmic jerking movements of muscles.
2. Focal epilepsy
These seizures originate in a specific area or focus of the brain. Focal seizures can be further classified into:
- Focal Aware Seizures ( simple partial seizures): These kinds of seizures occur without loss of consciousness. The individual remains aware of their surroundings but may experience unusual movements, sensations, or emotions.
- Focal Impaired Awareness Seizures complex partial seizures): These seizures are characterized by altered consciousness or awareness. The person may appear confused, disoriented, or engage in purposeless movements.
- Focal to Bilateral Tonic-Clonic Seizures: These begin as focal seizures initially, but later, they spread to involve both sides of the brain, leading to a generalized tonic-clonic seizure.
Causes
The causes of epilepsy can be different for each person. Some episodes of seizure activity can be linked to genetics, brain trauma, stroke, autoimmune disorders, metabolic issues, or infectious diseases, while others may have no identifiable causes.
Triggers
Some common triggers for seizures include:
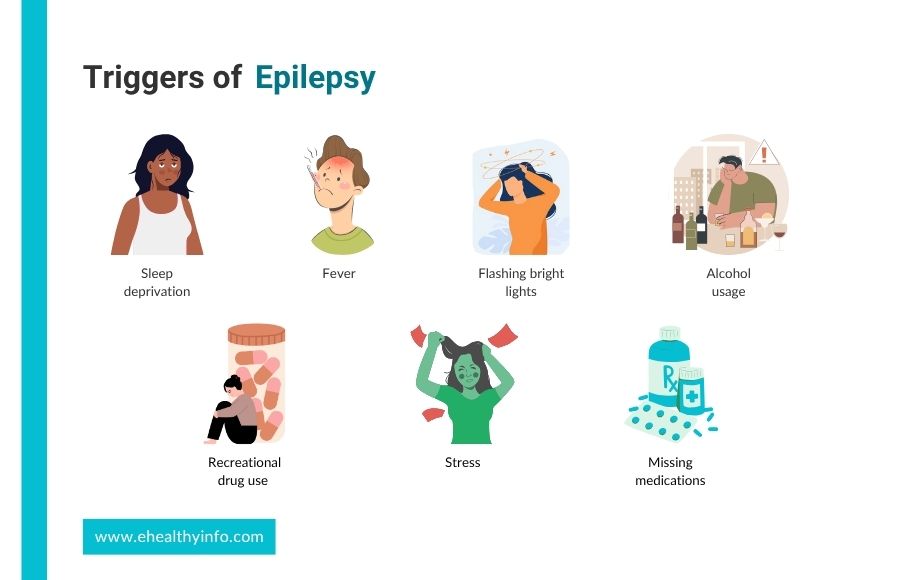
- Sleep deprivation
- Fever
- Flashing bright lights
- Alcohol Usage
- Recreational Drug use
- Stress
- Stress Missing medications for seizure
Signs and Symptoms of Epilepsy
Since seizure in epilepsy has varied presentations, it sometimes gets difficult to recognize one. Here are some of the ways seizures in epilepsy can present:

- Aura: Some people experience a warning sign or sensation before a seizure, known as an aura. This can vary widely among individuals, including feelings of Deja vu, strange smells or tastes, visual disturbances, or sudden emotional changes.
- Loss of Awareness: Many seizures involve a loss of awareness or consciousness. During this time, the person may appear to stare blankly into space, be unresponsive, or be unable to communicate.
- Uncontrollable Movements: Seizures often involve uncontrollable movements. These can vary greatly, from jerking motions in the arms and legs to more subtle twitching or repetitive movements. During these movements, one might bite their tongue, which needs immediate attention.
- Changes in Sensation: Some seizures may cause unusual sensations or feelings, such as tingling, numbness, fear, or panic.
- Loss of Control: In some cases, individuals may lose control of bodily functions, such as bladder or bowel control.
- Duration: Seizures typically last for a short time, usually only a few seconds to a few minutes. Prolonged seizures, or seizures that occur one after another without full recovery in between, are called status epilepticus and require immediate medical attention.
Diagnosis
The diagnosis of epilepsy will require a detailed history and neurological examination in the beginning. After that, your doctor will recommend various tests to diagnose it. Here is the overview of the diagnostic process:

1. Blood tests
Blood tests are performed to check for metabolic disorders, infections, or other medical conditions that can cause seizures. It will help to rule out all the other conditions that might present with seizure.
2. Electroencephalogram (EEG)
EEG is a critical diagnostic technique for epilepsy. It records the brain’s electrical activity through electrodes placed on the scalp. In epilepsy, EEG detects abnormal patterns like spikes and sharp waves, indicating potential seizure activity and pinpointing the location of seizure onset within the brain. There are different types of EEG studies, including routine EEG, ambulatory EEG, and video EEG monitoring in specialized units. These aid in capturing and analyzing brain activity over varying durations, allowing for accurate diagnosis and treatment planning.
3. Magnetic resonance imaging (MRI)
It is the preferred imaging modality for epilepsy evaluation due to its superior soft tissue contrast and ability to visualize detailed brain anatomy. It can detect a range of abnormalities, including mesial temporal sclerosis (MTS), neocortical dysplasia, brain tumors, and vascular malformations, all of which can cause seizures. Specific MRI protocols like T1-weighted, T2-weighted, FLAIR, and susceptibility-weighted imaging (SWI) are used to assess brain structure in relation to epilepsy.
4. Computed tomography (CT)
CT scans, while less sensitive than MRI, are sometimes used for emergency evaluations or when MRI is contraindicated. They can identify large lesions, hemorrhages, or calcifications associated with epilepsy. In certain cases, advanced imaging techniques such as positron emission tomography (PET) and single-photon emission computed tomography (SPECT) may be employed to characterize brain function further and localize the seizure focus, aiding in treatment decisions for individuals with epilepsy.
Treatment of Epilepsy
Treatment options for epilepsy can vary depending on factors such as the type of seizures, the underlying cause of epilepsy, and individual patient characteristics. Here are the main treatment options available for epilepsy:

1. Antiepileptic Medications (AEDs)
The most common and primary treatment for epilepsy involves taking AEDs. They work by stabilizing the electrical activity in the brain and reducing the likelihood of seizures. A wide range of AEDs are available, and the choice of AED depends on factors such as the type of seizures, patient age, potential side effects, and other medical conditions. Treatment often starts with a single AED at a low dose, which may be adjusted based on seizure control and tolerability. Some patients may require combination therapy with more than one AED to achieve optimal seizure management. Some of the common examples of AEDs are Carbamazepine (Tegretol), Valproate (Depakote), and Levetiracetam (Keppra).
-> Levetiracetam: Levetiracetam, marketed under Keppra, is a widely prescribed AED in the United States and globally due to its effectiveness and safety profile. Keppra is known for its broad-spectrum efficacy against various seizure types and is often used as adjunctive therapy alongside other AEDs. One of Keppra’s key advantages is its minimal side effect profile, with common side effects such as dizziness, somnolence, and irritability being generally mild and transient and not requiring monitoring of blood keppra levels for toxicity.
2. Ketogenic Diet
It is a diet high in fat, low in carbohydrates, and adequate protein. The ketogenic diet has shown efficacy in decreasing seizure episodes, particularly in children with epilepsy who do not respond well to medications. The diet induces a state of ketosis, where the body produces ketones from fat metabolism, which may have anticonvulsant effects on the brain. The ketogenic diet is typically supervised by a dietitian and requires strict adherence to specific macronutrient ratios.
3. Surgery
Surgical intervention may be considered for individuals with epilepsy who do not respond to medications or have seizures originating from a specific, identifiable area of the brain. Common surgical procedures for epilepsy include resective surgery (removal of the seizure focus), corpus callosotomy (cutting the corpus callosum to prevent seizure spread), and multiple subpial transections (to disrupt seizure pathways).
4. Vagus Nerve Stimulation (VNS)
VNS involves implanting a device that delivers electrical impulses to the vagus nerve in the neck. These impulses can help reduce seizure frequency and severity. VNS is considered for individuals with refractory epilepsy who are not candidates for surgery or have not responded well to medications alone.
5. Responsive Neurostimulation (RNS)
RNS is a newer treatment option that involves implanting a device directly into the brain to detect and respond to electrical activity associated with seizures. The device delivers targeted electrical stimulation to disrupt seizure activity before it spreads.
6. Lifestyle Modifications
Certain lifestyle changes can complement medical treatments and help manage epilepsy, such as getting adequate sleep, managing stress, avoiding alcohol and recreational drugs, and maintaining a regular schedule of meals and medications. Identifying and avoiding seizure triggers, such as specific foods, drinks, or environmental factors, can also be beneficial.
Cure of Epilepsy
While there is no definitive cure for epilepsy, treatments will help you control your symptoms.
Stopping anti-epileptic drugs
It’s important to continue your medications even if you have been seizure-free. Although you may feel fine, it’s crucial to consult your doctor before stopping AEDs. Typically, your doctor will gradually reduce the dosage and consider stopping your seizure medications entirely only after you have been seizure-free for a period of 2 to 4 years. If you have experienced only one seizure episode, your doctor might recommend discontinuing treatment if you remain seizure-free for 6 to 12 months.
There is a higher chance of remaining seizure-free without medications if:
- You had a few seizures before you started taking seizure medicine.
- Your seizures were controlled with just one type of medicine.
- You had normal results on a neurological examination.
- You had a normal EEG at the time of the diagnosis.
- Your CT scan or MRI results were normal.
Q. What to do after a seizure if you witness a seizure?
Ask the person’s name, place, time of the day, and about the seizure episode. If the person cannot answer the questions above, provide pertinent information and reassurance so they are not overwhelmed. Do not leave the person alone until they can talk, communicate well, and breathe normally.
Q. When should you call 911 or for emergency help?
If you see a seizure, be calm. However, do call for help if:
- The seizures last longer than 5 minutes.
- There are repeated seizures.
- The person had difficulty breathing.
- The seizures have occurred in water bodies such as lakes or swimming pools.
- The person is injured, pregnant, or sick.
- The person does not return to their usual after a seizure
- This is the person’s first seizure.
- The person asks for medical help.
Epilepsy and Exercise
The relationship between exercise and seizures in epilepsy is complex and requires individualized consideration. While regular physical activity like walking, swimming, or yoga can provide notable health benefits such as stress reduction and improved mood, it can also influence seizure activity positively or negatively.
Individuals with epilepsy need to engage in moderate-intensity activities while taking precautions to avoid overheating, dehydration, or excessive exertion, which can trigger seizures in some cases. Consulting with your doctor is essential to tailor exercise plans based on your medical history, seizure type, and medication regimen. Incorporating exercise into an overall epilepsy management strategy can enhance well-being while reducing the risk of seizures during physical activity.
1. Women and epilepsy
Epilepsy can uniquely impact women due to hormonal influences on seizure patterns, particularly during puberty, menstruation, pregnancy, and menopause. Hormonal fluctuations can affect seizure frequency and severity in some cases. Certain AEDs may also impact reproductive health, leading to menstrual irregularities, polycystic ovary syndrome (PCOS), or decreased bone density. Women with epilepsy require specialized care and considerations for contraception, fertility, and pregnancy, as managing medication safety and seizure control during pregnancy is crucial for maternal and fetal well-being.
2. Driving and Seizure Disorder
Being on the road alone can pose a risk to yourself and others if you have episodes of seizures. Seizures can make you unconscious or cause motor and visual impairment, which might be risky if you are on the road. A person with epilepsy must be seizure-free for a certain period to be eligible for a driver’s license. The seizure-free period varies from state to state, and you might need clearance from your doctor. You should refer to your state driving laws to see the latest rules and eligibility for driving if you have seizures.
Questions For Your Doctor
- How long should I continue my medication?
- When will I be able to drive?
- Should I breastfeed my child while I am on epilepsy medication?
- Are there some social support groups for those who have epilepsy?
- Do I need a wristband to notify others of my condition?
- Do I need a referral to a neurologist?
References
- http://Epilepsy | Epilepsy and Seizures | JAMA | JAMA Network
- https://www.cdc.gov/epilepsy/about/first-aid.htm
- https://www.epilepsy.com/what-is-epilepsy/seizure-triggers
- https://www.epilepsy.com/treatment/medicines/stopping-medication
- http://Epilepsy and Driving | Epilepsy Foundation
