Hepatitis A and E – Introduction, Similarities and Differences

Highlights of Hepatitis A and E
- Hepatitis A virus and Hepatitis E are the most common causes of acute liver inflammation worldwide.
- Symptoms of hepatitis A and E are similar. Common symptoms include fatigue, malaise, jaundice, nausea and vomiting, abdominal pain, pale-colored stool, and dark urine.
- The majority of the cases of hepatitis A and E require no specific treatment and resolve on their own. Rarely, Hepatitis A can lead to acute liver failure, especially in individuals with underlying liver conditions.
- A safe and effective vaccine is available to prevent Hepatitis A. This is recommended for high-risk individuals and travelers to endemic areas.
- Pregnant women are at a higher risk of severe complications from Hepatitis E.
What is Hepatitis A and Hepatitis B?
Hepatitis means inflammation of the liver. Although hepatitis can be caused due to heavy alcohol use, drugs, and toxins, it is most commonly caused by a virus. Viral hepatitis is caused by a group of viruses, namely hepatitis A, B, C, D, and E. Hepatitis A virus (HAV) and Hepatitis E virus (HEV) are the most common causes of acute hepatitis worldwide.
Hepatitis A
Hepatitis A virus commonly spreads through contaminated food and water or direct contact with an infected person. Once inside the body, the virus attacks normal liver cells, causing inflammation and damage. Hepatitis A is generally acute or short-lived, though in rare cases, it can lead to severe infection or liver failure. The virus is highly contagious and can be transmitted in two main ways: person-to-person contact, such as through close physical contact like sexual activities or shared needles, and through the oral-fecal route, usually via contaminated food or water.
Hepatitis E
Hepatitis E, a member of the Hepeviridae family, spreads primarily through the fecal-oral route and is called enteric hepatitis. The infection usually resolves on its own within two to six weeks.
Like Hepatitis A, Hepatitis E can be contracted by consuming contaminated food or water. Eating undercooked pork or organ meats from infected animals increases your chances of getting the virus from animal sources. Though less common, transmission can occur through blood transfusions, organ transplants from infected donors, or an infected mother to her child.
People at risk of Hepatitis A and E
Here are some groups of people who are at higher risk of getting Hepatitis A or Hepatitis E:
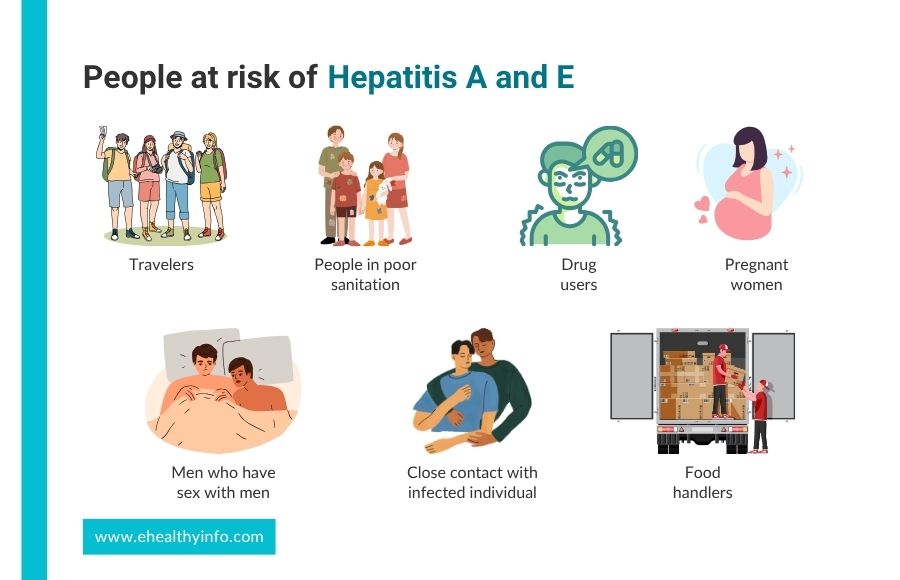
1. Travelers
If you travel to countries where these viruses are common, especially in areas with poor sanitation, you are more likely to be exposed and contract any of these viruses.
2. People in Poor Sanitation
Living in places without access to clean drinking water or proper waste management makes it easier for these viruses to spread.
3. Drug Users
Using drugs, whether injected or not, can increase your risk, especially if you’re in environments where hygiene and safety aren’t prioritized.
4. Men Who Have Sex With Men
You are at increased risk of getting Hepatitis A if you are a man who has sex with men.
5. Close Contact With Infected Individuals
Living with or caring for someone who has Hepatitis A puts you at higher risk, even before they start showing any symptoms.
6. Food Handlers
People who work with food are more likely to be exposed to Hepatitis A, especially if they come into contact with contaminated sources.
7. Pregnant Women
If you’re pregnant, there’s a higher risk of severe complications from Hepatitis E, particularly during the later stages of pregnancy.
Symptoms of Hepatitis A and E
Hepatitis A and Hepatitis E mostly present with similar symptoms; sometimes, the disease may develop without noticeable symptoms. The clinical presentation involves two phases: the prodromal phase followed by the icteric phase.
Prodromal phase: This phase lasts 3 to 10 days and is primarily characterized by malaise and myalgia. Other symptoms during this phase may include:

- Fever
- Anorexia
- Nausea and/or vomiting
- Abdominal pain
- Joint pain
Icteric phase: The next phase is the icteric phase, which may last up to 3 weeks. Symptoms during the icteric phase include:

- Yellowing of the skin and whites of the eyes
- Anorexia, nausea, and vomiting
- Dark urine and pale-colored stool
- Skin irritation and/or rash
- Abdominal pain and/or diarrhea
People who are more likely to experience severe disease from Hepatitis A and E include:
- Individuals with chronic liver disease, including Hepatitis B and C
- People living with HIV
- Pregnant women
Diagnosis of Hepatitis A and E
Initial Diagnostic Tests: Both Hepatitis A and E diagnoses involve blood tests to detect specific antibodies produced by your immune system in response to the viruses.
IgM antibodies
IgM antibodies are the first to emerge in response to Hepatitis A and E infections. They typically appear within the first week after infection, serving as an important marker for the body’s immune response. IgM antibodies indicate an acute infection and confirm recent exposure to either virus, helping healthcare providers diagnose the condition effectively.
IgG antibodies
IgG antibodies will develop as the infection progresses and your body starts to recover. These antibodies typically appear about 2 to 4 weeks after the onset of symptoms. IgG antibodies indicate that you have had a past infection or have developed immunity to the virus. This signifies that you are no longer infectious and have gained a certain level of protection against future infections.
Viral RNA
Detection of viral RNA is an important diagnostic tool for both Hepatitis A and E, complementing antibody testing. In Hepatitis A, the presence of Hepatitis A virus RNA can be identified using nucleic acid testing (NAT), which is particularly useful during the early stages of infection, often before antibodies are produced. Similarly, Hepatitis E virus RNA can also be detected through NAT, allowing for early diagnosis of the infection. This detection typically occurs shortly after infection, usually within the first week or two, before the immune response generates significant levels of antibodies. Identifying viral RNA is essential for diagnosing acute infections and can help distinguish Hepatitis A and E from other liver diseases. Viral RNA is used to monitor the viral load in patients, assess the severity of the infection, and guide treatment decisions.
Treatment of Hepatitis A and E
Both hepatitis A and E mostly resolve on their own within 4-8 weeks. Almost all cases of HAV and HEV are self-limiting in immunocompetent patients.

Supportive care rocks here. Both Hepatitis A and E typically require supportive care, as these infections are self-limiting and resolve on their own without specific antiviral medications. Adequate rest is crucial for helping your body recover from the infection. Drinking plenty of fluids can help prevent dehydration. Maintaining good hydration is essential, especially if symptoms like nausea and vomiting occur. You might need over-the-counter medications to alleviate specific symptoms, such as pain relievers for abdominal discomfort or fever reducers.
Monitoring for complications and hospitalization
In most cases, both Hepatitis A and E do not lead to chronic infection, and patients can expect a full recovery. However, monitoring may be necessary for those with pre-existing liver conditions or weakened immune systems to manage any complications. Severe cases, including fulminant hepatitis, require hospitalization. Antiviral drugs like ribavirin and interferon may also be used in cases of chronic hepatitis E. Although very rare, more serious cases may also require liver transplantation.
Complications of Hepatitis A and E
Complications from hepatitis A and E are uncommon. Certain populations, such as individuals with pre-existing liver diseases like chronic hepatitis B or C, pregnant women, and those with weakened immune systems, are at higher risk for severe complications from Hepatitis A and E. Some of the possible complications include:
1. Prolonged Symptoms
While most individuals recover fully, some people may experience prolonged symptoms such as fatigue, weakness, and jaundice that can last for weeks or even months after the initial infection. This post-viral fatigue can significantly impact daily life and requires time for recovery.
2. Chronic Liver Disease
Although chronic infection is rare for both Hepatitis A and E, individuals with existing liver problems may experience worsening of their condition. This can lead to complications like cirrhosis or liver cancer over time.
3. Acute Liver Failure
In rare cases, both Hepatitis A and E can lead to acute liver failure, a severe condition where the liver suddenly loses its ability to function. This can result in symptoms such as jaundice, confusion, and bleeding tendencies. Acute liver failure requires immediate medical attention and often leads to hospitalization.
4. Pregnancy Complications
Pregnancy poses unique risks when it comes to Hepatitis E, as infected pregnant women are at a significantly higher risk of developing severe complications, including acute liver failure. This increased susceptibility is particularly concerning during the third trimester, with the greatest likelihood of severe outcomes. Infections during pregnancy can lead to adverse effects for both the mother and the fetus, including the risk of stillbirth, premature delivery, and maternal mortality. The transmission of the virus from the mother to the fetus can also occur, potentially resulting in neonatal infection.
Prevention of Hepatitis A and E
1. Good Hygiene Practices
Both Hepatitis A and E are transmitted through the fecal-oral route, making good hygiene practices crucial. Regular handwashing with soap and water, especially after using the bathroom and before preparing or consuming food, can significantly reduce the risk of infection.
2. Safe Food and Water
Ensuring access to clean and safe drinking water is essential for preventing both Hepatitis A and E. Avoiding tap water in areas where the virus is common, drinking bottled or boiled water, and being cautious about ice made from unpurified water can help prevent infection. When eating, especially in areas where the viruses are endemic, opt for well-cooked foods and avoid raw or undercooked shellfish, fruits, and vegetables that cannot be peeled.
3. Travel Precautions
If you’re traveling to regions where Hepatitis A or E is common, take precautions by getting vaccinated ahead of time, practicing good hygiene, and being mindful of food and water safety. This is particularly important in developing countries where sanitation may be inadequate.
4. Avoiding Risky Behaviors
Reducing high-risk behaviors, such as sharing needles or engaging in unprotected sex with multiple partners, can help prevent Hepatitis A transmission, especially among men who have sex with men. Although Hepatitis E is less commonly transmitted through person-to-person contact, maintaining general safe practices is still advisable.
5. Vaccination
The most effective way to prevent Hepatitis A is through vaccination. The Hepatitis A vaccine is safe and effective and is recommended for all children aged 12-23 months. It is also recommended for individuals at higher risk, such as travelers to endemic areas, people with chronic liver diseases, and men who have sex with men. Although there is currently no vaccine for Hepatitis E, awareness of its prevention strategies remains important.
Hepatitis A Vaccine Schedule and Its Side Effects
In the US, there are now two registered single-antigen vaccinations. One year or older is the recommended age for the first dose of all inactivated hepatitis A vaccinations, authorized for intramuscular injection into the deltoid muscle in a two-dose regimen.
A 6-to-18-month delay between dosages one and two is normally recommended, although this can be extended to 4 or 5 years. Over-18-year-olds can receive the combination vaccine containing both HAV and HBV antigens. Three doses are given during primary immunizations in the first, first, and sixth months. Common side effects of the vaccine include fever, headache, tiredness, and soreness at the injection site.
Questions To Ask Your Doctor
- If I have been exposed to someone with Hepatitis A or E, what steps should I take?
- How long should I expect symptoms to last?
- Can I take over-the-counter drugs during hepatitis A and E?
- Are there any dietary restrictions?
- How often should I have follow-up appointments after recovering from Hepatitis A or E?
References
- Webb GW, Kelly S, Dalton HR. Hepatitis A and Hepatitis E: Clinical and Epidemiological Features, Diagnosis, Treatment, and Prevention. Clin Microbiol Newsl 2020;42:171. https://doi.org/10.1016/J.CLINMICNEWS.2020.10.001.
- Van Damme P, Pintó RM, Feng Z, Cui F, Gentile A, Shouval D. Hepatitis A virus infection. Nat Rev Dis Primers 2023;9. https://doi.org/10.1038/s41572-023-00461-2.
- Jeong SH, Lee HS. Hepatitis a: Clinical manifestations and management. Intervirology 2010;53:15–9. https://doi.org/10.1159/000252779.
- Waqar S, Sharma B, Koirala J. Hepatitis E. Treatment and Management of Tropical Liver Disease 2023:1–7. https://doi.org/10.1016/B978-0-323-87031-3.00010-X.
- Migueres M, Lhomme S, Izopet J. Hepatitis A: Epidemiology, High-Risk Groups, Prevention and Research on Antiviral Treatment. Viruses 2021;13:1900. https://doi.org/10.3390/v13101900.
- Hepatitis E | CDC Yellow Book 2024 [Internet]. wwwnc.cdc.gov. Available from: https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/hepatitis-e
- Hepatitis and reproduction. Fertil Steril 2008;90:S226–35. https://doi.org/10.1016/j.fertnstert.2008.08.040.
- Nelson NP, Link-Gelles R, Hofmeister MG, Romero JR, Moore KL, Ward JW, et al. Update: Recommendations of the Advisory Committee on Immunization Practices for Use of Hepatitis A Vaccine for Postexposure Prophylaxis and for Preexposure Prophylaxis for International Travel. MMWR Morb Mortal Wkly Rep 2018;67:1216–20. https://doi.org/10.15585/mmwr.mm6743a5.
- Mirazo S, Ramos N, Mainardi V, Gerona S, Arbiza J. Transmission, diagnosis, and management of hepatitis E: an update. Hepat Med 2014;6:45. https://doi.org/10.2147/HMER.S63417.
- Miller JM, Binnicker MJ, Campbell S, Carroll KC, Chapin KC, Gilligan PH, et al. A Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2018 Update by the Infectious Diseases Society of America and the American Society for Microbiologya. Clinical Infectious Diseases 2018;67:e1–94. https://doi.org/10.1093/cid/ciy381.
- Hepatitis E | CDC Yellow Book 2024 [Internet]. wwwnc.cdc.gov. Available from: https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/hepatitis-e
- Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recommendations and Reports 2021;70:1–187. https://doi.org/10.15585/mmwr.rr7004a1.
- Aslan AT, Balaban HY. Hepatitis E virus: Epidemiology, diagnosis, clinical manifestations, and treatment. World J Gastroenterol 2020;26:5543–60. https://doi.org/10.3748/wjg.v26.i37.5543.
- Abravanel F, Lhomme S, Marion O, Péron JM, Kamar N, Izopet J. Diagnostic and management strategies for chronic hepatitis E infection. Expert Rev Anti Infect Ther 2023;21:143–8. https://doi.org/10.1080/14787210.2023.2166932.
- Shingina A, Mukhtar N, Wakim-Fleming J, Alqahtani S, Wong RJ, Limketkai BN, et al. Acute Liver Failure Guidelines. American Journal of Gastroenterology 2023;118:1128–53. https://doi.org/10.14309/ajg.0000000000002340.
- Kamar N, Izopet J, Pavio N, Aggarwal R, Labrique A, Wedemeyer H, et al. Hepatitis E virus infection. Nat Rev Dis Primers 2017;3:17086. https://doi.org/10.1038/nrdp.2017.86.
- Sarkar M, Brady CW, Fleckenstein J, Forde KA, Khungar V, Molleston JP, et al. Reproductive Health and Liver Disease: Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2021;73:318–65. https://doi.org/10.1002/hep.31559.
- Liang Y, Zhang J, Luo D, Cheng L, Wang Y. Deregulation of immune response contributing to fulminant hepatitis in HEV infected pregnant women. J Med Virol 2024;96. https://doi.org/10.1002/jmv.29639.
- Wu C, Wu X, Xia J. Hepatitis E virus infection during pregnancy. Virol J 2020;17:73. https://doi.org/10.1186/s12985-020-01343-9.
- Van Damme P, Pintó RM, Feng Z, Cui F, Gentile A, Shouval D. Hepatitis A virus infection. Nat Rev Dis Primers 2023;9:51. https://doi.org/10.1038/s41572-023-00461-2.
- Letafati A, Taghiabadi Z, Roushanzamir M, Memarpour B, Seyedi S, Farahani AV, et al. From discovery to treatment: tracing the path of hepatitis E virus. Virol J 2024;21:194. https://doi.org/10.1186/s12985-024-02470-3.
- Bhandari P, Brett C, Batool A, Sapra A. Hepatitis A Vaccine. Pediatric Vaccines and Vaccinations: A European Textbook: Second Edition 2023:115–25. https://doi.org/10.1007/978-3-030-77173-7_12.
Return to Home
