Iron deficiency anemia (IDA) is an anemia where your body doesn’t have enough iron to make healthy red blood cells. This is the most common form of anemia, affecting almost 30% of people worldwide, making it a major public health issue. [1]
IDA develops when you lack enough iron in your body, which is required to form hemoglobin, a part of red blood cells. Hemoglobin carries oxygen and removes carbon dioxide from the body. Therefore, a lack of iron in the body affects the proper functioning of your overall body as it does not get enough oxygen to work with. [2]
IDA usually occurs when there is a lack of iron in the diet, a loss of iron, or a problem with iron absorption in the body.
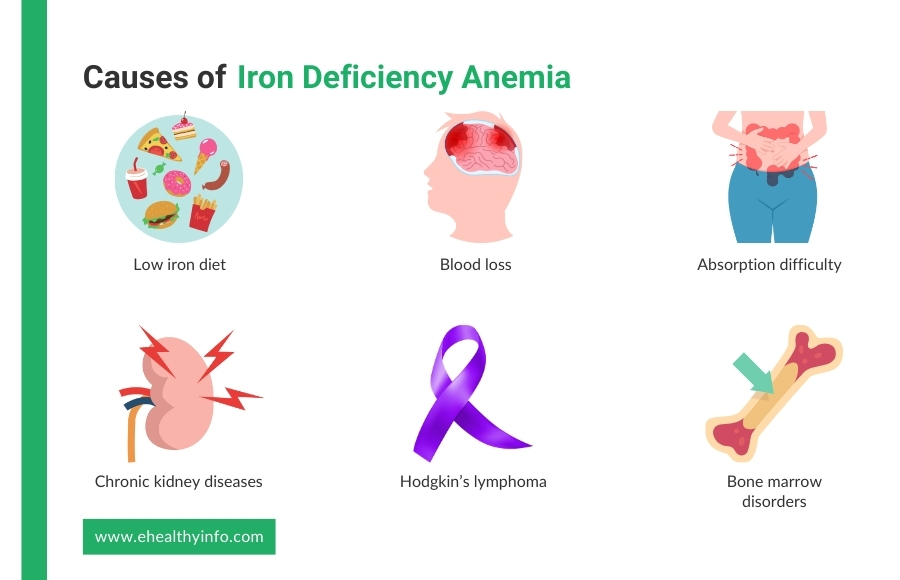
Your body gets iron from the food you eat. If your diet doesn’t have enough iron-rich foods, your iron levels can drop over time. This is common if you eat mostly plant-based foods, avoid meat or poultry, or follow a restrictive diet such as a vegan or vegetarian diet without proper substitutes. The recommended daily dietary intake of iron is around 8 mg for an adult male and 18 mg for an adult female. However, only 1 mg of iron is absorbed for every 10 to 20 mg of iron ingested. [3-4]
Iron is lost when you lose blood. If you lose more iron than your body can replace, you can develop IDA. Common causes of blood loss include gastrointestinal (GI) bleeding, urinary tract bleeding, heavy menstrual bleeding, traumatic injury, and surgeries, etc. People who regularly use aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) are prone to GI bleeding, leading to anemia. [5]
Even if you eat enough iron, sometimes your body might not be able to absorb it well. This means that you could be getting enough iron from your diet, but it isn’t reaching your bloodstream to be used by your cells. This could be because of conditions like celiac disease, Crohn’s disease, or ulcers, as they can damage the lining of your intestine, making it harder for you to absorb iron from food. Other such conditions can be surgical procedures. [6]
Other less common causes of IDA include chronic kidney diseases (CKD), cancer such as Hodgkin’s lymphoma, bone marrow disorders, intravascular hemolysis, heart failure, parasitic infections like hookworm, long-term illnesses such as HIV/AIDS, hepatitis B and C, obesity, etc. These conditions may directly or indirectly affect your body’s ability to produce red blood cells from the body, leading to anemia. [7-8]
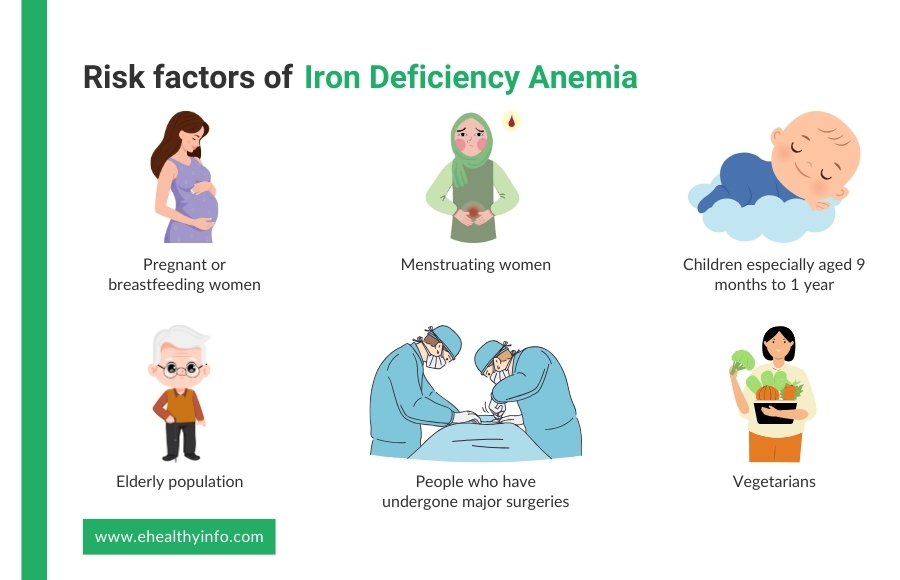
Certain people are at increased risk of developing iron-deficiency anemia. People at higher risk for iron-deficiency anemia include:
IDA can cause several symptoms because your body isn’t getting enough oxygen due to low iron levels. The symptoms, however, may be very mild in the beginning and later become worse. One of the most common signs is extreme fatigue and weakness. You may feel unusually tired, even after enough rest, or have trouble completing daily tasks. This happens because your red blood cells, which carry oxygen, are reduced in number and unable to do their job efficiently, leaving you feeling drained and low on energy. [10]
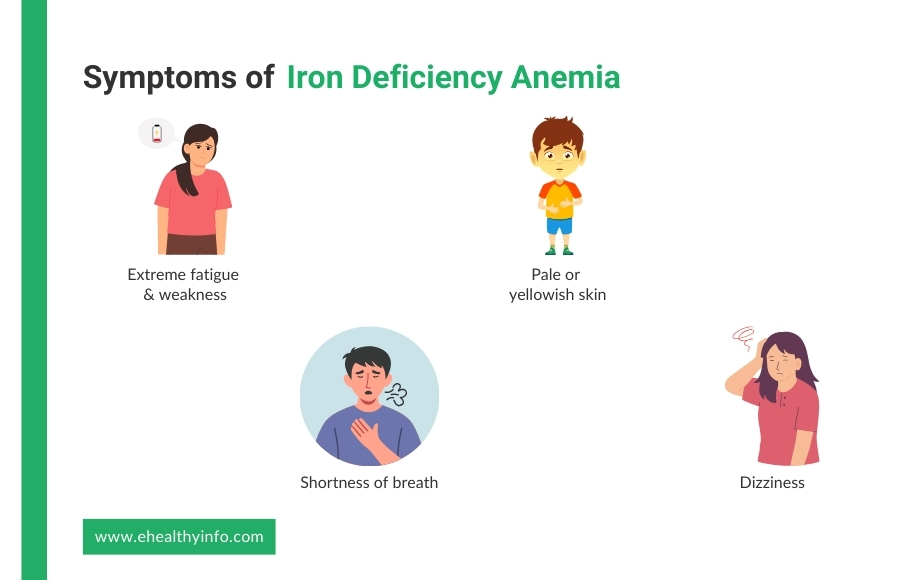
Other symptoms of IDA include pale or yellowish skin, shortness of breath, and dizziness. [11] As your iron levels drop, your skin might appear paler than usual, and you may notice you feel winded or out of breath after activities that wouldn’t usually tire you out. Some people also experience headaches, cold hands or feet, increased heart rate, and a taste for unusual stuff like ice, wood, and soil, a condition called pica. [12]
The most common tests for diagnosing IDA are:
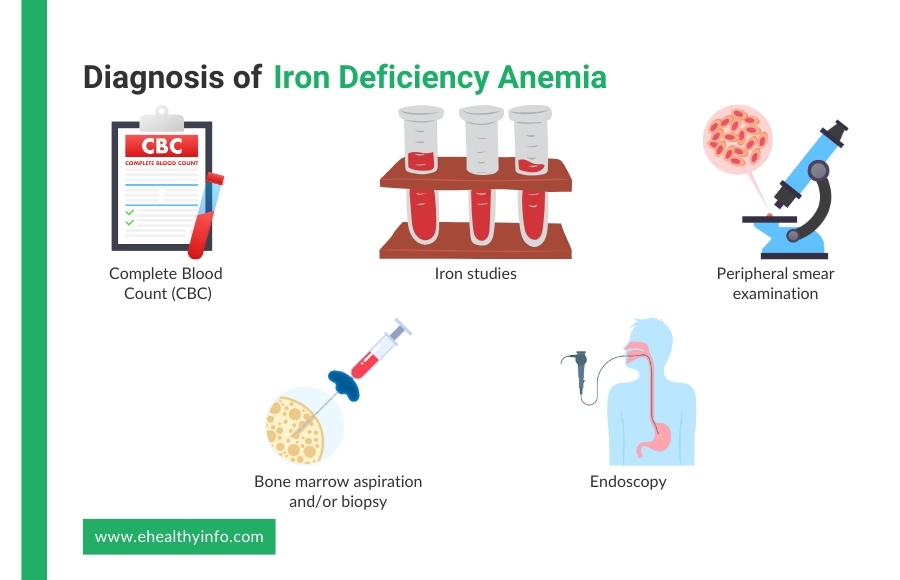
This test measures the number of red blood cells in your blood. In IDA, your red blood cell count, hemoglobin, and hematocrit (the percentage of blood made up of red blood cells) will be lower than normal. [13]
Iron studies are a group of blood tests used to assess the amount of iron in your body and how well it uses and stores it. Common tests in iron studies include the serum iron test, which measures the level of iron circulating in your blood, and the serum ferritin test, which shows how much iron is stored in your body. The Total Iron-Binding Capacity (TIBC) test also measures how much transferrin (the protein that carries iron) can bind with iron. These iron studies help your doctor determine whether you have iron deficiency, its severity, and any underlying causes for the imbalance. [14]
A peripheral smear examination is a laboratory test where a blood sample is spread on a microscope slide and examined for abnormalities in the shape, size, and number of blood cells. In IDA, the peripheral smear may show microcytic (smaller-than-normal) red blood cells that are also hypochromic (pale due to less hemoglobin). This examination helps identify the characteristics of your red blood cells. It can reveal clues about the underlying cause of anemia, such as whether it’s due to iron deficiency, a chronic disease, or another condition. [6]
Bone marrow aspiration and biopsy are procedures used to collect a small sample of bone marrow to check for abnormalities in blood cell production. In cases of IDA, these tests can show reduced iron stores in the marrow, confirming the lack of sufficient iron for red blood cell production. While it is not typically the first test for diagnosing IDA, bone marrow examination is helpful in complex cases or when other underlying conditions, such as bone marrow disorders, must be ruled out. These procedures help provide a clearer picture of the cause of anemia when standard tests are inconclusive. [15]
Endoscopy is a procedure used to check for hidden causes of IDA, especially when internal bleeding is suspected. It helps your doctor to look inside your digestive tract to find problems like stomach ulcers, inflammation, or bleeding in the intestines. There are two main types: upper endoscopy, where a small camera is passed through your mouth to check your stomach and upper intestines, and colonoscopy, where a camera is inserted through the rectum to examine the colon. Endoscopy is usually recommended if your anemia is unexplained or if your doctor suspects slow, long-term blood loss from your digestive system. [6]
The treatment of IDA focuses on restoring iron levels and addressing the underlying cause of the deficiency. The main approaches include:
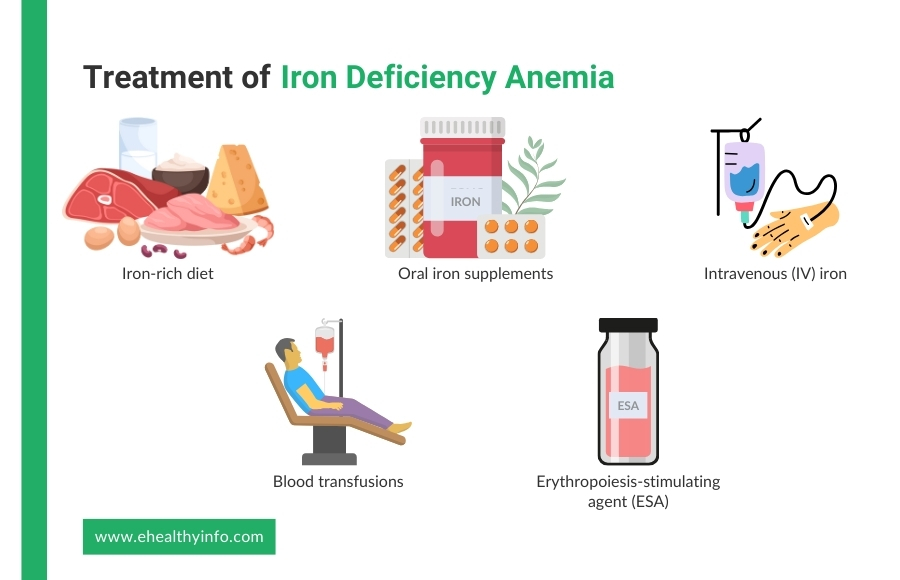
Eating foods high in iron helps replenish your body’s iron stores. Good sources include red meat, poultry, fish, leafy green vegetables (like spinach), beans, lentils, nuts, and iron-fortified cereals. Pairing these with vitamin C-rich foods (like citrus fruits or tomatoes) helps improve iron absorption. [14]
If diet alone is insufficient, you might need oral iron supplements (such as ferrous sulfate, ferrous fumarate, or ferrous gluconate). These are usually taken on an empty stomach with vitamin C for better absorption. But they come with side effects like constipation, nausea, or stomach upset. Because of these side effects, alternate-day dosing has been suggested if someone is not tolerating iron supplements. Alternate-day dosing was found to have greater efficacy with iron absorption and hemoglobin improvement. [16]
If you cannot tolerate oral iron, you have absorption issues and severe anemia, and iron injections might be recommended. It helps to replenish iron absorption quickly. However, it is more costly than oral iron and has a small risk of allergic reactions. [17]
The American Society of Hematology recommends transfusing blood only for those with severe and symptomatic anemia who cannot maintain blood pressure. This means it is reserved for a severe case only. [14]
ESAs are sometimes used to treat IDA, especially in patients with CKD, cancer, or other conditions that affect red blood cell production. ESAs, such as erythropoietin and darbepoetin alfa, help stimulate the bone marrow to produce more red blood cells, reducing the need for blood transfusions. However, ESAs are usually given alongside iron supplements because the body needs enough iron to support increased red blood cell production. These medications are typically used in cases where anemia is severe, persistent, or not improving with iron therapy alone. [18]
Milder cases of IDA have no complications. But when left untreated, iron-deficiency anemia can cause severe complications such as:
When iron levels are low, your heart has to work harder to pump oxygen-poor blood. Over time, this extra stress can cause irregular heartbeats, an enlarged heart, or even heart failure in severe cases. If you already have a heart condition, you are at a higher risk of complications of IDA. [19]
Pregnant women need extra iron to support the baby’s growth. If IDA is left untreated during pregnancy, it increases the risk of premature birth, low birth weight, and developmental problems in the baby. It can cause complications during delivery and increase the risk of postpartum depression in mothers. [20–21]
Iron is essential for brain development in children. If a child has untreated IDA, they may have slower growth, learning difficulties, and problems with memory or concentration. This can affect their school performance and overall development. [20]
You can prevent IDA by ensuring you get enough iron in your diet. Eating iron-rich foods and pairing them with vitamin C helps your body absorb iron better. At the same time, try to limit tea and coffee during meals since they can block iron absorption. Parasitic infections, like hookworms, can cause blood loss and lead to anemia, so maintaining good hygiene, drinking clean water, and deworming treatments can help. Some foods are fortified with iron to ensure people get enough from their diet. Regular check-ups, treating any health issues that cause blood loss, and taking iron supplements if needed are good ways to keep your iron levels healthy and prevent anemia. [22]
Screening for IDA in pregnancy is important to ensure the health of both the mother and the baby. Pregnant women are at higher risk for IDA due to increased iron requirements to support the growing fetus and the expanded blood volume. Routine screening typically involves blood tests such as hemoglobin level and serum ferritin to assess iron stores. Screening for IDA is generally done during the first prenatal visit and again around the 24th to 28th week of pregnancy. Early detection allows timely treatment with iron supplements or dietary changes to prevent complications. Pregnant women, particularly those with a history of heavy menstrual periods or poor nutritional intake, should be regularly monitored throughout their pregnancy to ensure they maintain adequate iron levels. [23]
Adolescents with IDA are likely to experience depression and anxiety. Studies have shown a clear link between low iron levels and mental health problems, as iron is essential for brain function and the production of mood-regulating chemicals like serotonin and dopamine. [24] When iron levels drop, the brain may not function properly, leading to feelings of sadness, fatigue, and difficulty concentrating. [11] Research also suggests that adolescents, especially those from multiracial backgrounds, may have higher rates of depression and anxiety if they have IDA. Since teenagers are already going through many physical and emotional changes, untreated iron deficiency can make these struggles even worse. [24]
Pica is a condition where people crave and eat non-food items like dirt, ice, or chalk, and it often occurs in individuals with IDA. While IDA is the most common cause, pica can also occur due to other nutritional deficiencies, such as zinc or calcium. In some cases, pica may be linked to mental health disorders like obsessive-compulsive disorder or schizophrenia. It can also be seen in pregnancy, where cravings for non-food items like ice (a form of pica called pagophagia) are relatively common. The exact reason this happens is unclear, but it’s believed the body may crave these non-food items to cope with nutrient deficiencies. People with IDA may experience pica as a response to low iron levels, which can lead to further complications if left untreated. [12]