Melanoma Explained – Symptoms, Stages, Treatment & Prevention

Highlights of Melanoma
- Melanoma is a type of skin cancer that is less common than other forms of skin cancer but is dangerous. This is due to its ability to spread quickly to other body parts.
- Fair skin, family history of melanoma, significant sun exposure or sunburns, a high number of moles, and male gender all increase your risk of developing melanoma.
- Key warning signs of melanoma include irregular or poorly defined borders, variegated colors, lesions larger than 6 mm, and any changes in shape or size over time.
- The earlier melanoma is diagnosed, the higher the chance of successful treatment.
- Protecting your skin from UV radiation is the most effective way to reduce your risk. Use broad-spectrum sunscreen, wear protective clothing, and avoid tanning beds.
What is Melanoma?
Melanoma is a type of skin cancer that is derived from melanocytes. Melanocytes are special skin cells that secrete melanin, the dark pigment responsible for giving the skin its characteristic color.
Melanoma is less common in general populations when compared to other forms of skin cancers, but it is common in white populations. However, melanoma is dangerous, particularly because of its ability to quickly spread to other parts of the body. Fair-skinned and light-haired people with high UV exposure are at increased risk of developing melanoma.
Risk Factors and Causes of Melanoma
Melanoma has been linked to several potential causes, such as:
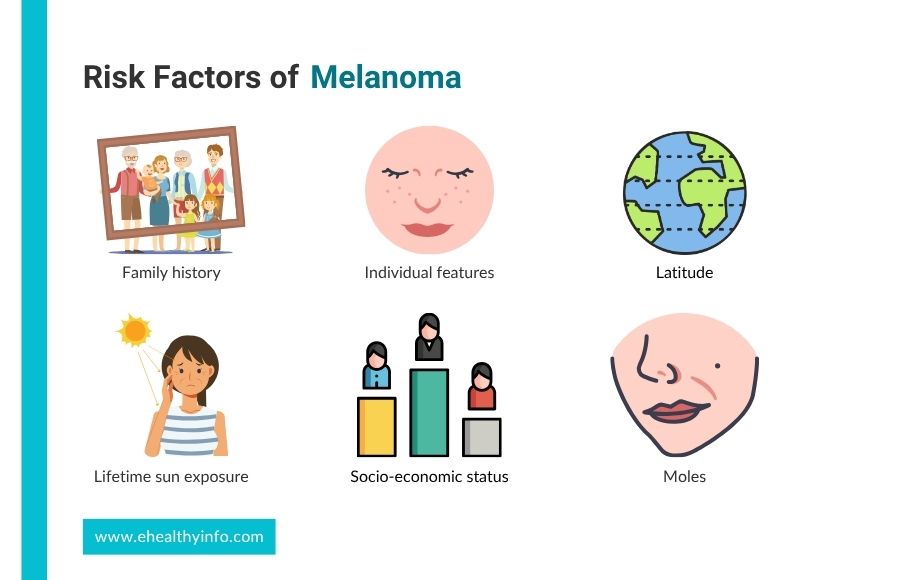
1. Family History
If someone in your family, like a parent or sibling, has had melanoma, you’re more likely to get it too. 5 to 10% of the cases of melanoma are known to have a family history, and if you have one family member with melanoma then you are 2.2 times more likely than general people to get it.
2. Individual Features
Blue eyes, red or blonde hair, fair skin tone, history of sunburns, and freckles are known high-risk factors for causing melanoma.
3. Lifetime Sun Exposure
Lifetime sun exposure is a key risk factor for melanoma, as the more time your skin is exposed to the sun, the more UV radiation it absorbs, leading to cumulative damage. Each time your skin is in the sun without protection, the UV rays can harm the DNA in your skin cells. Over the years, even without frequent sunburns, small, repeated exposures—like tanning or spending time outdoors without sunscreen add up, increasing your risk.
4. Latitude
If you live in places closer to the equator or at higher elevations, you’re exposed to stronger UV rays, which increases your risk of developing melanoma. At higher altitudes, the air is thinner, so UV rays can penetrate more easily, and near the equator, the sun’s rays are more direct.
5. Moles
If you have a lot of moles or unusual-looking moles, your risk of melanoma goes up. Changes in shape, size, or the color of the moles are considered risks for having melanoma.
6. Socioeconomic Status
At the time of diagnosis, a lower socioeconomic position may be associated with a more advanced condition. Patients of low socioeconomic class perceive a lower risk of melanoma, are less knowledgeable about the disease, and follow fewer preventative measures.
Symptoms of Melanoma
Melanoma can appear on any area of the body. Melanomas are more common on the trunk in cases of males and on lower limbs in cases of females. Melanoma can present over the skin in many different ways. The typical signs of melanoma are often described by the ABCDE mnemonic. The ABCDEs of melanoma include:

1. A – Asymmetry
One half of the mole or skin spot doesn’t match the other half. If you draw a line through the middle of a mole, both sides should look the same. In melanoma, one-half is often uneven or irregular in shape.
2. B – Border
Melanomas tend to have irregular, scalloped, or poorly defined edges. If the borders of your mole are jagged or blurred, it’s something to watch out for, as healthy moles usually have smooth and clear borders.
3. C – Color
Normal moles are usually a single shade of brown or black. Melanomas often have a variety of colors, including different shades of brown, black, tan, or even red, blue, or white. A mole with multiple colors or unusual tones is a warning sign.
4. D – Diameter
Melanomas are often larger than 6 millimeters in diameter (about the size of a pencil eraser), although they can be smaller when first detected.
5. E – Evolving
Look out for any mole that changes over time, whether in size, shape, color, or elevation—or any new symptoms like bleeding, itching, or crusting. Evolution is a key sign that something may be wrong.
Other Warning Signs
If a mole or spot becomes painful, itchy, or tender, it may indicate a problem. Bleeding, oozing, or crusting from a mole is also a red flag, as healthy moles don’t typically do this. Another sign is any new growth or mole that suddenly appears on your skin, especially if it looks unusual. Also, pay attention to changes in texture; if a mole becomes rough, scaly, or raised, it could be a sign of melanoma.
Diagnosis of Melanoma
Examining the area of skin under question is the most important aspect of diagnosing melanoma.

1. Dermatoscopy
Dermatoscopy is a non-invasive tool doctors use to examine your skin more closely. It’s like a special magnifying glass that helps your doctor see deeper into a mole or spot, looking for patterns, colors, and other details that aren’t visible to the naked eye. This tool helps in deciding whether a mole might be melanoma.
2. Skin Biopsy and Histopathology
Skin biopsy and histopathology are the key steps to confirm melanoma. If your doctor suspects melanoma after examining your skin, they’ll remove a small part (or all) of the mole in a biopsy. This sample is sent to a lab where specialists look at the cells under a microscope to check if they are cancerous. This is the most definitive way to diagnose melanoma.
3. Imaging
These tests might be used if there’s a concern that melanoma has spread to other parts of your body. Common imaging techniques include ultrasound, which uses sound waves to create images of soft tissues; CT scans, which provide detailed cross-sectional images of the body; and MRIs, which use magnetic fields to create detailed images of organs and tissues. These scans help doctors check if the cancer has affected organs like your lymph nodes, lungs, or liver.
Treatment of Melanoma
Treating involves several strategies depending on the stage and location of the cancer and patient-specific factors. These treatment options vary depending on the stage and specific characteristics of the disease. Various treatment options involve:

Surgical
Surgery is the primary treatment for early-stage melanoma. During this procedure, the surgeon removes the melanoma along with a margin of healthy skin surrounding it to ensure the complete removal of cancerous cells. If the melanoma is thicker or has spread to nearby lymph nodes, a wider excision may be necessary. Sometimes, a sentinel lymph node biopsy is performed to check if the cancer has spread. This involves removing and examining the nearest lymph node to the melanoma. Successful surgical intervention can lead to excellent outcomes, especially when the melanoma is diagnosed at an early stage.
Immunotherapy
Immunotherapy enhances the body’s natural immune response to recognize and fight melanoma cells. One of the most common types of immunotherapy is checkpoint inhibitors, which help to remove the “brakes” on the immune system, allowing it to attack cancer more effectively. Drugs such as pembrolizumab and nivolumab have shown significant success in treating advanced melanoma. Patients often experience durable responses, meaning that the benefits can last for a long time, even after treatment has stopped.
Targeted Therapy
This therapy focuses on specific genetic mutations that are present in melanoma cells. For instance, many melanomas have mutations in the BRAF gene, making them susceptible to drugs like vemurafenib and dabrafenib, which specifically target and inhibit the growth of these mutated cells. Targeted therapy is particularly beneficial for patients with advanced melanoma and can be combined with other treatments to enhance efficacy.
Chemotherapy
Chemotherapy involves the use of powerful drugs to kill rapidly dividing cells, including cancer cells. Although it is less commonly used for melanoma today due to the effectiveness of immunotherapy and targeted therapy, chemotherapy can still play a role in certain cases, particularly when the cancer has spread significantly. While chemotherapy can be effective, it may also come with significant side effects.
Radiation Therapy
Radiation therapy utilizes high-energy rays to target and destroy cancer cells, often used when surgery isn’t an option or to treat areas of the body where melanoma has recurred. This treatment can help shrink tumors or relieve pain caused by advanced melanoma. Radiation may be used as an adjunct therapy after surgery to eliminate remaining cancer cells, thereby reducing the risk of recurrence. Patients undergoing radiation therapy typically receive several sessions over a set period, and the side effects can vary, but many find that it effectively helps manage their disease.
Prognosis of Melanoma
The prognosis of melanoma depends primarily on the stage at diagnosis. Early-stage melanomas have a favorable prognosis, with five-year survival rates exceeding 90%. Prognosis worsens with regional spread and is poor for distant metastasis, though advancements in immunotherapy and targeted therapy have improved outcomes in advanced cases.
Other factors influencing prognosis include tumor thickness and ulceration. Younger patients and females generally have a better prognosis than older patients and males. Overall, health and genetic factors have a role in prognosis. Similarly, the effectiveness of initial and subsequent treatments greatly influences the prognosis. Patients responding well to therapies such as immunotherapy or targeted therapy often experience prolonged survival and improved quality of life.
Prevention of Melanoma
Here are four effective strategies for melanoma prevention:

1. Sun Protection
Protecting your skin from the sun is crucial. When outdoors, use sunscreen with at least SPF 30, applying it generously and reapplying every two hours, especially after swimming or sweating. Wearing protective clothing, such as long sleeves and wide-brimmed hats, can also shield your skin from harmful UV rays. Additionally, seek shade during peak sun hours, typically between 10 AM and 4 PM, when the sun’s rays are the strongest.
2. Avoid Tanning Beds
Tanning beds can expose your skin to high levels of UV radiation, increasing your risk of developing melanoma and other skin cancers.
3. Regular Skin Checks
Performing regular self-examinations of your skin can help you spot any new or changing moles or spots early on. Familiarize yourself with the appearance of your moles and look for any changes in size, shape, color, or texture.
4. Awareness of Risk Factors
Being aware of the factors that increase your risk for melanoma, such as a family history of skin cancer, having many moles, or a history of sunburns, can help you take preventive measures.
Questions To Ask Your Doctor
- Are there any genetic factors that could affect my prognosis or treatment?
- How often should I schedule follow-up visits after treatment?
- How likely is melanoma to recur after treatment?
- What are the signs and symptoms of melanoma recurrence I should watch for?
- How can I access support groups or resources for patients with melanoma?
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018;68:7–30. https://doi.org/10.3322/caac.21442.
- Papageorgiou C, Apalla Z, Manoli S-M, Lallas K, Vakirlis E, Lallas A. Melanoma: Staging and Follow-Up. Dermatol Pract Concept 2021;11:e2021162S-e2021162S. https://doi.org/10.5826/dpc.11S1a162S.
- Leiter U, Eigentler T, Garbe C. Epidemiology of Skin Cancer. Sunlight, Vitamin D and Skin Cancer, New York, NY: Springer New York; 2014, p. 120–40. https://doi.org/10.1007/978-1-4939-0437-2_7.
- Olsen CM, Pandeya N, Neale RE, Law MH, Whiteman DC. Phenotypic and genotypic risk factors for invasive melanoma by sex and body site. British Journal of Dermatology 2024. https://doi.org/10.1093/bjd/ljae297.
- Kwa M, Ravi M, Elhage K, Schultz L, Lim HW. The risk of ultraviolet exposure for melanoma in Fitzpatrick skin types I– <scp>IV</scp> : A 20‐year systematic review with meta‐analysis for sunburns. Journal of the European Academy of Dermatology and Venereology 2024. https://doi.org/10.1111/jdv.20316.
- Crombie IK. Variation of melanoma incidence with latitude in North America and Europe. Br J Cancer 1979;40:774–81. https://doi.org/10.1038/bjc.1979.260.
- Swetter SM, Tsao H, Bichakjian CK, Curiel-Lewandrowski C, Elder DE, Gershenwald JE, et al. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol 2019;80:208–50. https://doi.org/10.1016/j.jaad.2018.08.055.
- Longo C, Pampena R, Moscarella E, Chester J, Starace M, Cinotti E, et al. Dermoscopy of melanoma according to different body sites: Head and neck, trunk, limbs, nail, mucosal and acral. Journal of the European Academy of Dermatology and Venereology 2023;37:1718–30. https://doi.org/10.1111/jdv.19221.
- Xing Y, Bronstein Y, Ross MI, Askew RL, Lee JE, Gershenwald JE, et al. Contemporary Diagnostic Imaging Modalities for the Staging and Surveillance of Melanoma Patients: a Meta-analysis. JNCI Journal of the National Cancer Institute 2011;103:129–42. https://doi.org/10.1093/jnci/djq455.
- Rutkowski P, Zdzienicki M, Nowecki ZI, Van Akkooi ACJ. Surgery of primary melanomas. Cancers (Basel) 2010;2:824–41. https://doi.org/10.3390/cancers2020824.
- Long G V, Luke JJ, Khattak MA, de la Cruz Merino L, Del Vecchio M, Rutkowski P, et al. Pembrolizumab versus placebo as adjuvant therapy in resected stage IIB or IIC melanoma (KEYNOTE-716): distant metastasis-free survival results of a multicentre, double-blind, randomised, phase 3 trial. Lancet Oncol 2022;23:1378–88. https://doi.org/10.1016/s1470-2045(22)00559-9.
- Luke JJ, Rutkowski P, Queirolo P, Del Vecchio M, Mackiewicz J, Chiarion-Sileni V, et al. Pembrolizumab versus placebo as adjuvant therapy in completely resected stage IIB or IIC melanoma (KEYNOTE-716): a randomised, double-blind, phase 3 trial. The Lancet 2022;399:1718–29. https://doi.org/10.1016/s0140-6736(22)00562-1.
- Henderson MA, Burmeister BH, Ainslie J, Fisher R, Di Iulio J, Smithers BM, et al. Adjuvant lymph-node field radiotherapy versus observation only in patients with melanoma at high risk of further lymph-node field relapse after lymphadenectomy (ANZMTG 01.02/TROG 02.01): 6-year follow-up of a phase 3, randomised controlled trial. Lancet Oncol 2015;16:1049–60. https://doi.org/10.1016/s1470-2045(15)00187-4.
- Burmeister BH, Henderson MA, Ainslie J, Fisher R, Di Iulio J, Smithers BM, et al. Adjuvant radiotherapy versus observation alone for patients at risk of lymph-node field relapse after therapeutic lymphadenectomy for melanoma: a randomised trial. Lancet Oncol 2012;13:589–97. https://doi.org/10.1016/s1470-2045(12)70138-9.
- Goldinger SM, Buder-Bakhaya K, Lo SN, Forschner A, McKean M, Zimmer L, et al. Chemotherapy after immune checkpoint inhibitor failure in metastatic melanoma: a retrospective multicentre analysis. Eur J Cancer 2022;162:22–33. https://doi.org/10.1016/j.ejca.2021.11.022.
- Bliley R, Avant A, Medina TM, Lanning RM. Radiation and Melanoma: Where Are We Now? Curr Oncol Rep 2024;26:904–14. https://doi.org/10.1007/s11912-024-01557-y.
- An S, Kim K, Moon S, Ko K-P, Kim I, Lee JE, et al. Indoor Tanning and the Risk of Overall and Early-Onset Melanoma and Non-Melanoma Skin Cancer: Systematic Review and Meta-Analysis. Cancers (Basel) 2021;13:5940. https://doi.org/10.3390/cancers13235940.
