Highlights of Osteoarthritis
- Osteoarthritis is the most common joint condition, affecting the hands, knees, neck, hips, and lower back.
- Osteoarthritis is one of the major causes of disability in older people, but it can also occur in the young population.
- Osteoarthritis can cause symptoms such as pain, stiffness, limited range of motion, and swelling in a joint.
- Joint replacement surgery can be an option for individuals with severe joint pain, deformity, and dysfunction when conservative treatments are no longer effective.
- PRP injections are an emerging treatment for osteoarthritis, using the patient’s own blood to promote healing.
What is Osteoarthritis (OA) ?
Osteoarthritis (OA) is the most common type of arthritis and occurs when the cartilage in joints breaks down, causing pain, stiffness, and difficulty moving. It usually affects the knees, hips, hands, and spine. [1] Worldwide, about 528 million people have OA in the year 2019, with about 60% of them being women. [2] In the United States, about 53 million adults have some form of arthritis, making it a major cause of disability in older people. [3]
Types of Osteoarthritis
Osteoarthritis can be classified into two types depending on the cause.
1. Primary osteoarthritis
It is the most common type of OA. It develops over time. It is believed to be caused due to wear and tear of the joint throughout your life. There is no predisposing trauma or disease in primary osteoarthritis.
2. Secondary osteoarthritis
This type of osteoarthritis occurs due to a preexisting joint disease. Predisposing conditions include congenital joint disorders, inflammatory arthritis, osteoporosis, metabolic disorders like hemochromatosis, injury, and trauma.
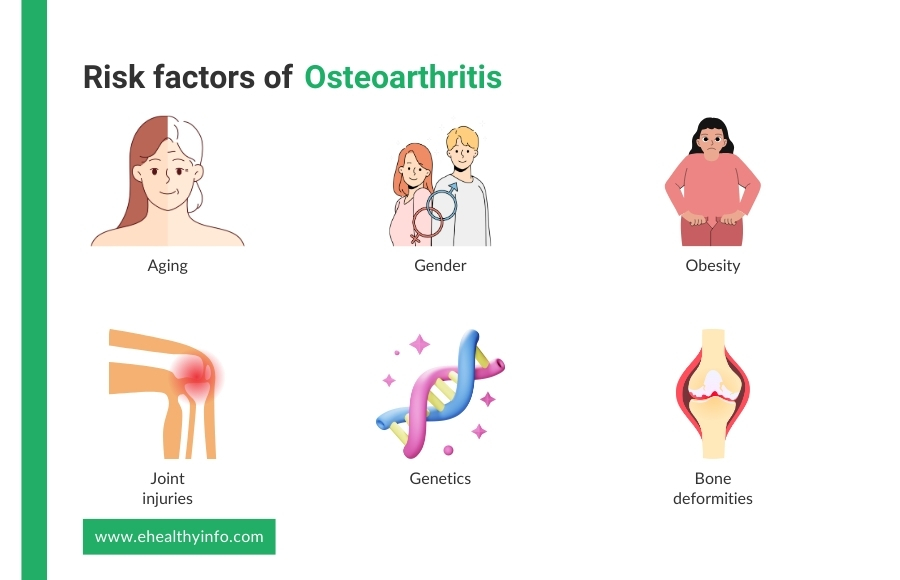
Causes and Risk Factors of Osteoarthritis
Although the exact cause of osteoarthritis is not yet known, certain risk factors increase your risk of developing it:
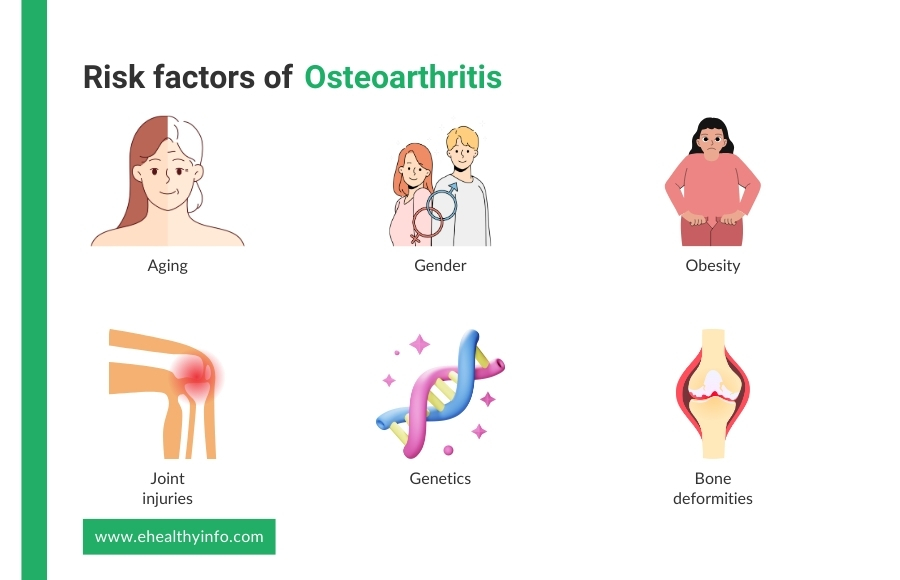
- Aging: As people age, the cartilage that cushions joints naturally deteriorates, leading to OA. [4]
- Gender: The cases of hip, knee, and hand OA are found to be higher in women than men, and the incidence of the condition increases around menopause. This has been attributed to the effect of decreasing levels of hormones in women. [4]
- Joint injuries: Injuries from sports, accidents, or repetitive stress can damage the cartilage and increase the risk of OA. Among all the joints, the knee is one of the most commonly injured joints. Thus, the prevalence of OA is also higher among women. [4]
- Obesity: Obesity that is defined by a body mass index of more than 30kg/m2 is strongly associated with knee OA. Excess body weight adds extra stress to weight-bearing joints like the knees and hips, accelerating cartilage breakdown. [4]
- Genetics: A family history of OA can increase an individual’s risk, suggesting a genetic predisposition. It accounts for 60% of hand and hip OA, while it is the cause of 40% of cases of knee OA. [4]
- Bone deformities: Some people are born with malformed joints, such as varus or valgus deformities or defective cartilage, which can lead to OA.
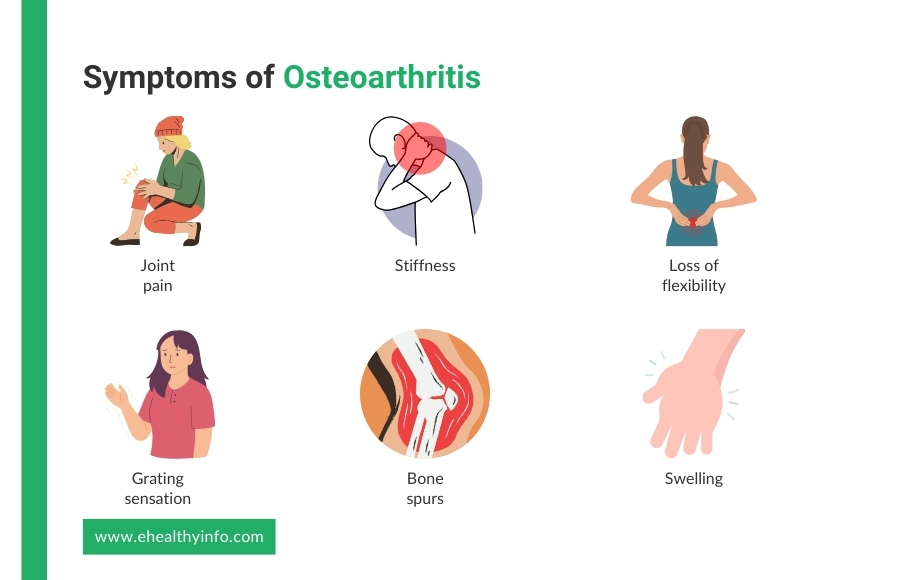
Symptoms of Osteoarthritis
OA symptoms can vary in severity and often develop gradually. Common symptoms include:
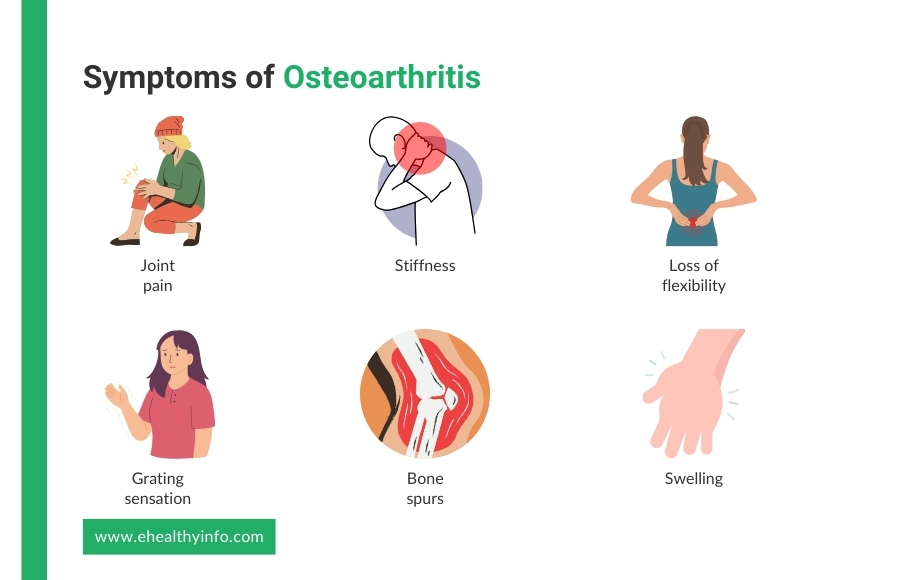
1. Joint pain
Pain in the affected joints during or after movement is a hallmark of osteoarthritis. This pain often worsens with activity and may improve with rest but can eventually become constant as the disease progresses. [5]
2. Stiffness
You may notice joint stiffness, especially upon waking up in the morning or after periods of inactivity, such as sitting for a long time. This stiffness typically eases within 30 minutes of movement but can recur throughout the day. [6]
3. Loss of flexibility
Reduced range of motion is common, making it difficult for you to move the joint fully. This loss of flexibility can interfere with simple movements like bending, reaching, or grasping objects. [7]
4. Grating sensation
You may feel a grating or hear a crackling sound (crepitus) when moving the joint. This occurs due to the rough surfaces of the cartilage and bone rubbing against each other. [7]
5. Bone spurs
Extra bits of bone, known as osteophytes or bone spurs, can form around the affected joint. These spurs can cause additional pain and limit joint movement. [6,7]
6. Swelling
You may see occasional swelling around the joint due to inflammation. This swelling can cause further discomfort and stiffness, and it may fluctuate depending on activity levels and other factors. [7]
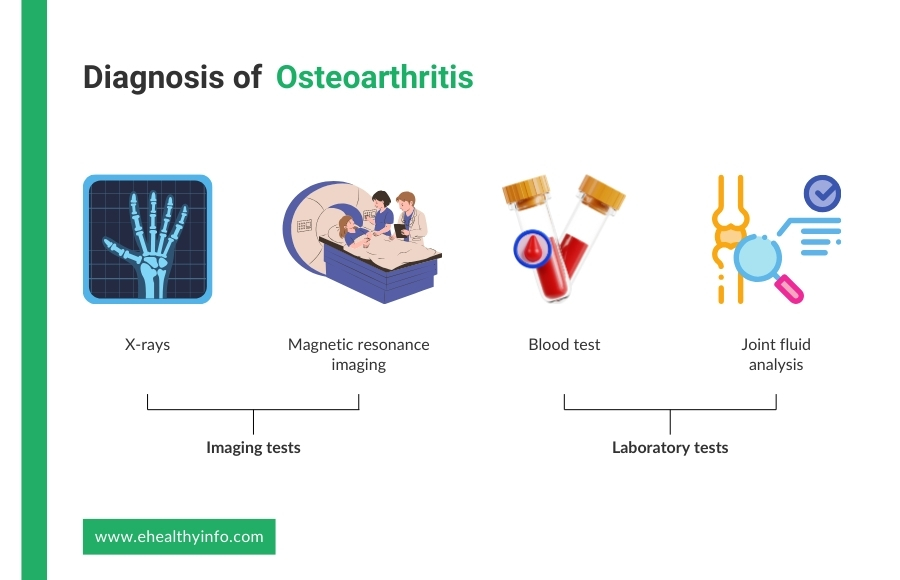
Diagnosis of Osteoarthritis
Diagnosis of OA is primarily done with the help of presenting symptoms and imaging. Some of the diagnostic modalities for OA are:
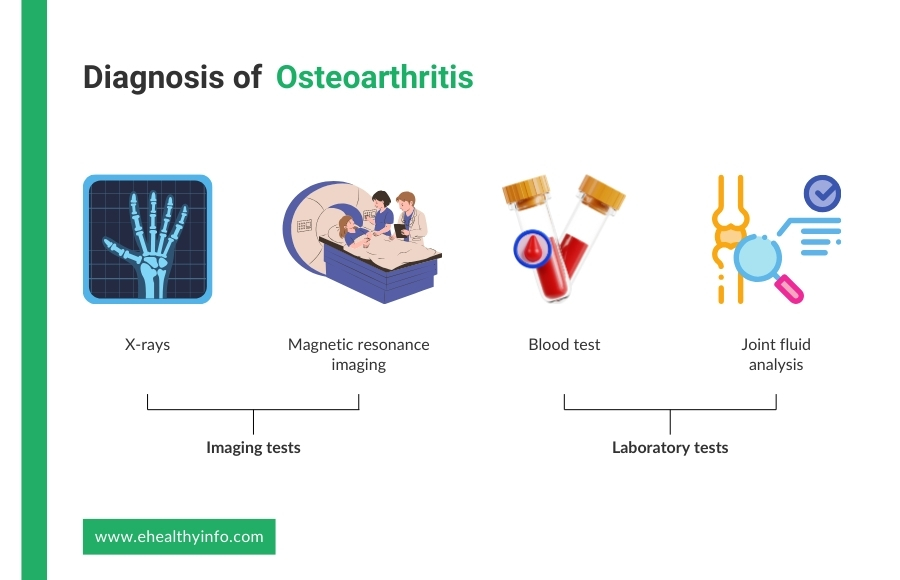
Imaging tests for osteoarthritis
- X-rays: X-rays are commonly used to diagnose OA. They can reveal joint space narrowing, the presence of bone spurs, and other changes in the bone structure that are indicative of OA. [8]
- Magnetic Resonance Imaging (MRI): MRI is not routinely performed for OA, but it helps by providing more detailed images of the joint’s soft tissues, including cartilage, tendons, and ligaments. It is particularly useful in early OA detection and in cases where the diagnosis is uncertain or more complex. [8,9]
Laboratory tests for osteoarthritis
- Blood tests: While there are no specific blood tests for OA, they can help rule out other types of arthritis, such as rheumatoid arthritis or gout, which can present similar symptoms. Inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate can also be used in severe cases, though OA is not related to systemic inflammation. [10]
- Joint fluid analysis: In some cases, your doctor may extract a sample of synovial fluid from the affected joint using a needle. Analyzing this fluid can help exclude other inflammatory joint conditions, such as infection or gout. [11,12]
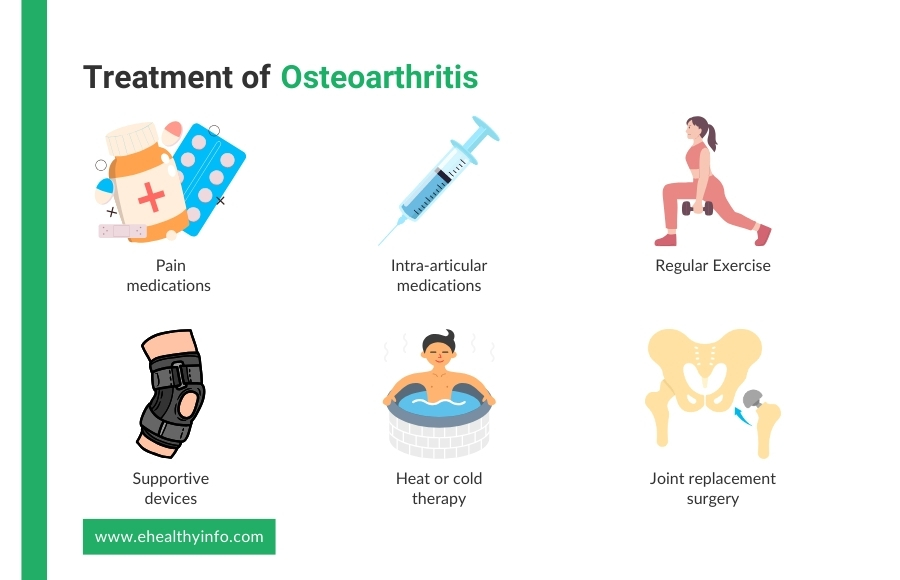
Treatment of Osteoarthritis
The principles of management and treatment of osteoarthritis include several key objectives: reducing pain and other symptoms, improving joint movement and function, stopping the progression of the disease, and maintaining quality of life. Here are the treatment modalities for OA:
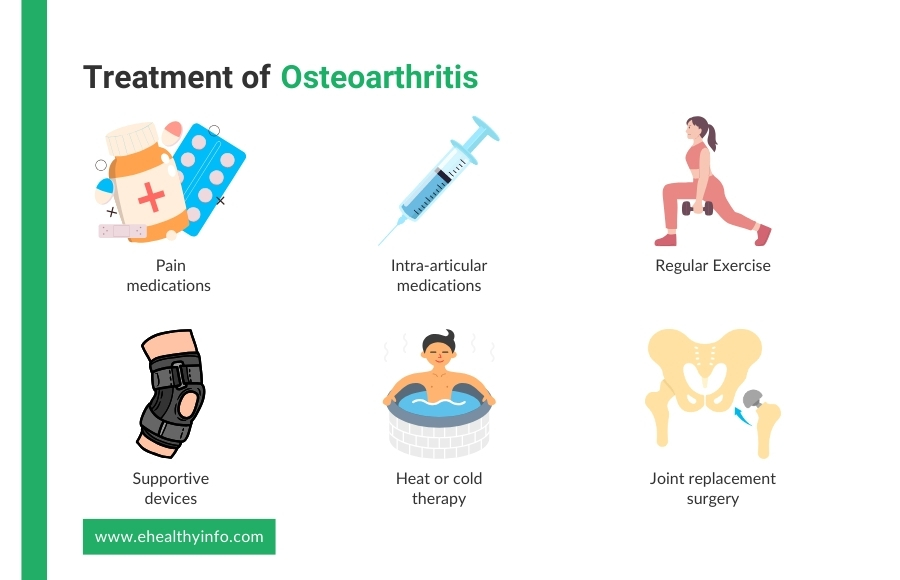
1. Pain medications
You can use over-the-counter pain medication to relieve your pain. They can be either topical, like creams, ointments, and patches, or oral. Oral anti-inflammatory medications like NSAIDs can also be helpful. [13]
2. Intra-articular medications
Intra-articular injections of corticosteroids and hyaluronic acids can also be effective, especially for acute pain.[13]
3. Exercise
Exercise helps improve symptoms like pain and stiffness alongside increasing flexibility. Low-impact exercises are particularly helpful. Stretching and strengthening exercises are also equally beneficial. Your doctor may recommend a physiotherapist to help you find the best exercises. [14]
4. Supportive devices
Wearing aids, knee braces, or shoe inserts take pressure off affected joints. These devices, therefore, help with the symptoms. Simple steps such as wearing comfortable shoes can also make a considerable difference.[15]
5. Heat or cold therapy
Heat therapy uses methods like heating pads or warm baths, while cold therapy uses ice packs or cold compresses. Heat helps to relax and loosen tissues, increase blood flow, and alleviate stiffness and chronic pain. Cold therapy, on the other hand, reduces inflammation, numbs pain, and decreases swelling, especially during flare-ups. [16]
6. Joint replacement surgery
Joint replacement therapies offer a solution for individuals experiencing severe joint pain and dysfunction when conservative treatments are no longer effective. Total joint replacement, such as hip or knee arthroplasty, involves surgically removing the damaged joint and replacing it with an artificial implant. This procedure aims to relieve pain, restore function, and improve quality of life by providing a new, smooth surface for joint movement. Partial joint replacement, where only the damaged portion of the joint is replaced, is another option that may be suitable for some patients. These therapies can significantly reduce pain and enhance mobility, allowing you to return to daily activities and improve your overall well-being. However, candidates for joint replacement typically undergo a thorough evaluation to ensure the procedure is appropriate based on their overall health, activity level, and specific joint damage. [17,18]
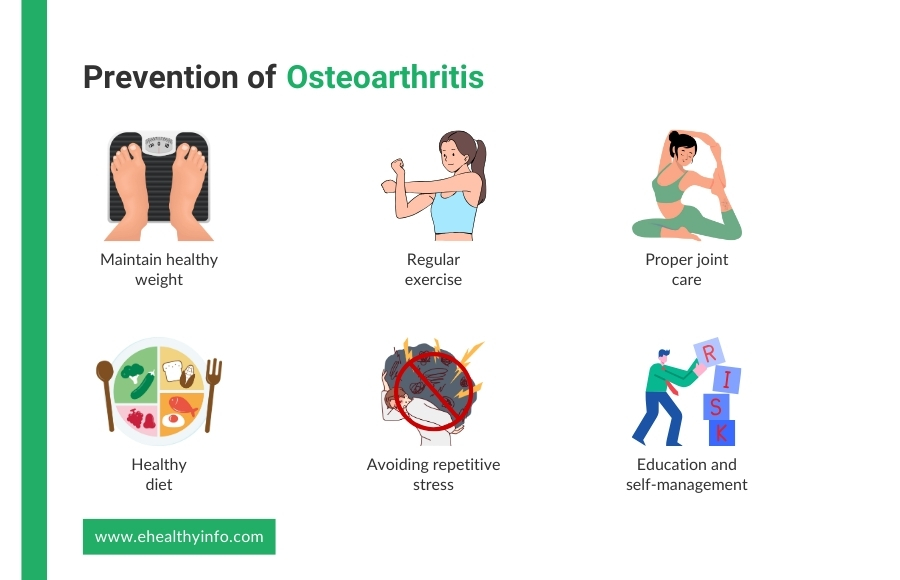
Prevention of Osteoarthritis
It is not possible to prevent osteoarthritis altogether. However, a healthy lifestyle and certain other factors can reduce your likelihood of developing or progressing OA. Some preventive measures include:
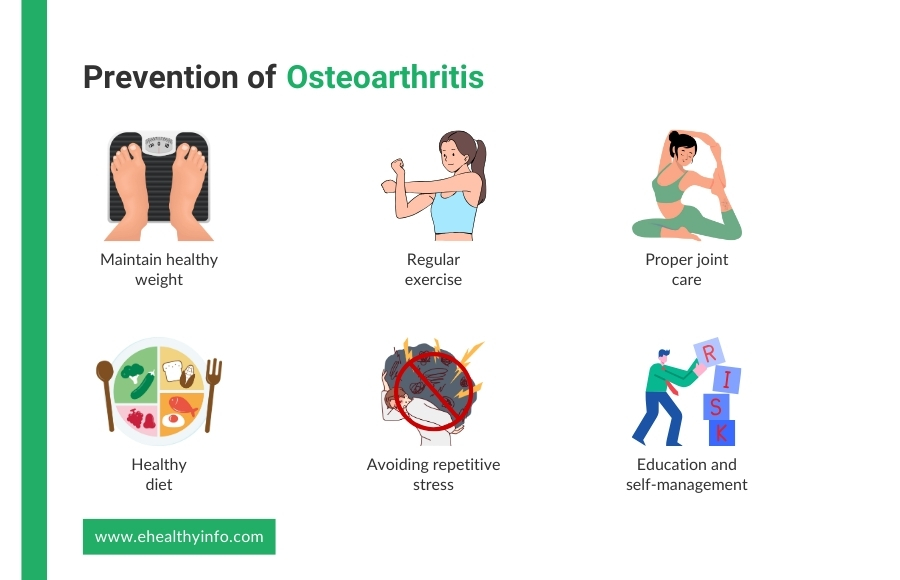
1. Maintain a healthy weight
Excess weight puts added stress on weight-bearing joints, particularly the knees and hips. Achieving and maintaining a healthy weight can significantly reduce the risk of OA. [19]
2. Regular exercise
Engaging in low-impact exercises like swimming, cycling, and walking helps to strengthen the muscles around the joints, improve flexibility, and maintain overall joint function. Strengthening exercises can also support joint stability. [20]
3. Proper joint care
Using proper techniques during physical activities and sports can help prevent joint injuries. Employing correct posture and body mechanics in daily activities also contributes to joint health. [20]
4. Healthy diet
A balanced diet rich in nutrients, including omega-3 fatty acids, vitamins C and D, and antioxidants, supports joint health and reduces inflammation. [20]
5. Avoiding repetitive stress
Minimizing repetitive stress and overuse of joints, especially in occupations or activities that place high demands on specific joints, can help prevent OA.
6. Education and self-management
Educating patients about the risk factors for developing osteoarthritis can significantly reduce the risk. [21]
Platelet-rich plasma (PRP) Injection for Osteoarthritis
PRP injection is an emerging treatment for osteoarthritis, and it uses the patient’s own blood to promote healing. The process involves drawing blood, centrifuging it to concentrate the platelets, and then injecting the PRP into the affected joint. Platelets contain growth factors and proteins that support tissue repair and regeneration. [22]This treatment aims to reduce pain and improve joint function by leveraging the body’s natural healing mechanisms. PRP injections are considered a promising option for managing osteoarthritis symptoms, though more research is needed to understand their long-term efficacy. [22,23]
Questions to Ask Your Doctor
- What exercises will benefit osteoarthritis?
- Will I have a normal life after developing osteoarthritis?
- Does surgery cure osteoarthritis?
- What natural therapies can I try to help with my joint function?
- What should I do if my symptoms suddenly worsen or if I experience new symptoms?
References
- Hall M, van der Esch M, Hinman RS, Peat G, de Zwart A, Quicke JG, et al. How does hip osteoarthritis differ from knee osteoarthritis? Osteoarthritis Cartilage 2022;30:32–41. https://doi.org/10.1016/J.JOCA.2021.09.010.
- Osteoarthritis n.d. https://www.who.int/news-room/fact-sheets/detail/osteoarthritis (accessed July 29, 2024).
- Fallon EA, Boring MA, Foster AL, Stowe EW, Lites TD, Odom EL, et al. Prevalence of Diagnosed Arthritis — United States, 2019–2021. MMWR Morb Mortal Wkly Rep 2023;72:1101–7. https://doi.org/10.15585/MMWR.MM7241A1.
- Palazzo C, Nguyen C, Lefevre-Colau MM, Rannou F, Poiraudeau S. Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med 2016;59:134–8. https://doi.org/10.1016/J.REHAB.2016.01.006.
- Perrot S, Anne-Priscille T. Pain in osteoarthritis from a symptom to a disease. Best Pract Res Clin Rheumatol 2023;37:101825. https://doi.org/10.1016/J.BERH.2023.101825.
- Ebell MH. Osteoarthritis: Rapid Evidence Review. Am Fam Physician 2018;97:523–6.
- Abhishek A, Doherty M. Diagnosis and Clinical Presentation of Osteoarthritis. Rheumatic Disease Clinics of North America 2013;39:45–66. https://doi.org/10.1016/J.RDC.2012.10.007.
- Mourad C, Vande Berg B. Osteoarthritis of the hip: is radiography still needed? Skeletal Radiol 2023;52:2259. https://doi.org/10.1007/S00256-022-04270-8.
- Wang X, Oo WM, Linklater JM. What is the role of imaging in the clinical diagnosis of osteoarthritis and disease management? Rheumatology 2018;57:iv51–60. https://doi.org/10.1093/RHEUMATOLOGY/KEX501.
- Woodell-May JE, Sommerfeld SD. Role of Inflammation and the Immune System in the Progression of Osteoarthritis. Journal of Orthopaedic Research® 2020;38:253–7. https://doi.org/10.1002/JOR.24457.
- Oliviero F, Scanu A, Galozzi P, Ramonda R. Synovial Fluid Analysis to Identify Osteoarthritis. Journal of Visualized Experiments 2022;2022. https://doi.org/10.3791/64351.
- Monibi F, Roller BL, Stoker A, Garner B, Bal S, Cook JL. Identification of Synovial Fluid Biomarkers for Knee Osteoarthritis and Correlation with Radiographic Assessment. Journal of Knee Surgery 2016;29:242–7.
- Brophy RH, Fillingham YA. AAOS Clinical Practice Guideline Summary: Management of Osteoarthritis of the Knee (Nonarthroplasty), Third Edition. Journal of the American Academy of Orthopaedic Surgeons 2022;30:e721–9. https://doi.org/10.5435/JAAOS-D-21-01233.
- Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage 2019;27:1578–89. https://doi.org/10.1016/j.joca.2019.06.011.
- Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis & Rheumatology 2020;72:220–33. https://doi.org/10.1002/art.41142.
- Yıldırım N, Filiz Ulusoy M, Bodur H. The effect of heat application on pain, stiffness, physical function and quality of life in patients with knee osteoarthritis. J Clin Nurs 2010;19:1113–20. https://doi.org/10.1111/j.1365-2702.2009.03070.x.
- Lützner J, Kasten P, Günther K-P, Kirschner S. Surgical options for patients with osteoarthritis of the knee. Nat Rev Rheumatol 2009;5:309–16. https://doi.org/10.1038/nrrheum.2009.88.
- Grayson CW, Decker RC. Total Joint Arthroplasty for Persons With Osteoarthritis. PM&R 2012;4. https://doi.org/10.1016/j.pmrj.2012.02.018.
- Roos EM, Arden NK. Strategies for the prevention of knee osteoarthritis. Nat Rev Rheumatol 2016;12:92–101. https://doi.org/10.1038/nrrheum.2015.135.
- Marriott KA, Birmingham TB. Fundamentals of osteoarthritis. Rehabilitation: Exercise, diet, biomechanics, and physical therapist-delivered interventions. Osteoarthritis Cartilage 2023;31:1312–26. https://doi.org/10.1016/j.joca.2023.06.011.
- Whittaker JL, Runhaar J, Bierma-Zeinstra S, Roos EM. A lifespan approach to osteoarthritis prevention. Osteoarthritis Cartilage 2021;29:1638–53. https://doi.org/10.1016/j.joca.2021.06.015.
- Meheux CJ, McCulloch PC, Lintner DM, Varner KE, Harris JD. Efficacy of Intra-articular Platelet-Rich Plasma Injections in Knee Osteoarthritis: A Systematic Review. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2016;32:495–505. https://doi.org/10.1016/j.arthro.2015.08.005.
- Xiong Y, Gong C, Peng X, Liu X, Su X, Tao X, et al. Efficacy and safety of platelet-rich plasma injections for the treatment of osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Front Med (Lausanne) 2023;10. https://doi.org/10.3389/fmed.2023.1204144.