
Polycystic ovary syndrome (PCOS) is a hormonal disorder affecting females of reproductive age. It occurs when your ovaries produce an excess of hormones called androgens. These androgens create an imbalance in your other reproductive hormones, leading you to have various symptoms like irregularity in menstruation and hirsutism, along with the development of cysts in your ovaries. It is estimated to affect up to 10% of women worldwide, making it one of the most prevalent endocrine disorders in this population.
Numerous risk factors elevate the likelihood of developing polycystic ovary syndrome. These factors include genetic predisposition, obesity, insulin resistance, and hormonal imbalances. Understanding these influences is crucial for detecting and effectively managing this complex condition.
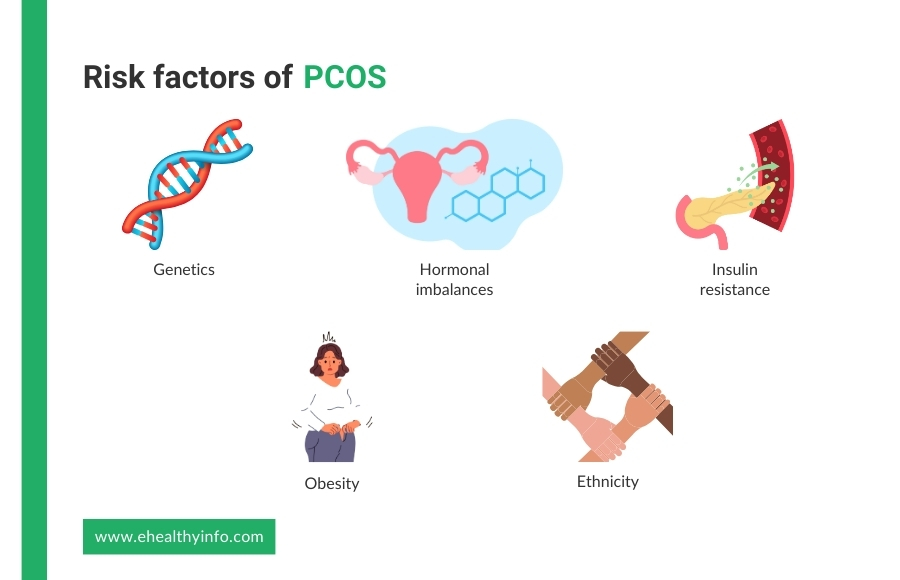
Family history plays a significant role in developing polycystic ovary syndrome. If you have someone with a first-degree relative, such as a mother or sister, who has PCOS, then you are at higher risk of developing the condition itself. This suggests a genetic predisposition to polycystic ovary syndrome.
Polycystic ovary syndrome is marked by elevated levels of androgens, such as testosterone, in the blood. These high levels of androgens can impair the functioning of the ovaries and lead to the development of cysts.
Insulin resistance is closely linked to polycystic ovary syndrome and can lead to increased insulin in the blood. Increased insulin, in turn, stimulates the ovaries to produce more androgens, disrupting the normal hormonal balance and contributing to the symptoms of polycystic ovary syndrome.
Obesity is strongly associated with PCOS. Excess body fat, particularly abdominal fat, can exacerbate insulin resistance and increase the production of androgens, further contributing to the hormonal imbalances seen in polycystic ovary syndrome.
PCOS affects women of all ethnicities, but some groups may be at higher risk than others. Studies have found that women of South Asian, Middle Eastern, and Hispanic descent may have a higher prevalence of polycystic ovary syndrome compared to women of other ethnic backgrounds.
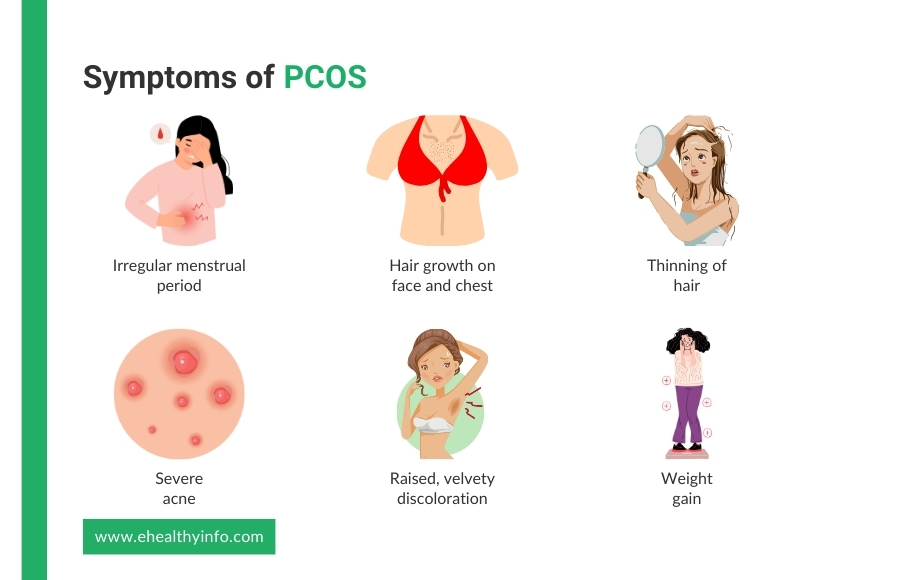
The most common signs and symptoms of polycystic ovary syndrome are:
Polycystic ovary syndrome is not just limited to its symptoms. It is also linked with an increased risk of developing other health conditions. Here are some of the disease conditions commonly associated with PCOS.
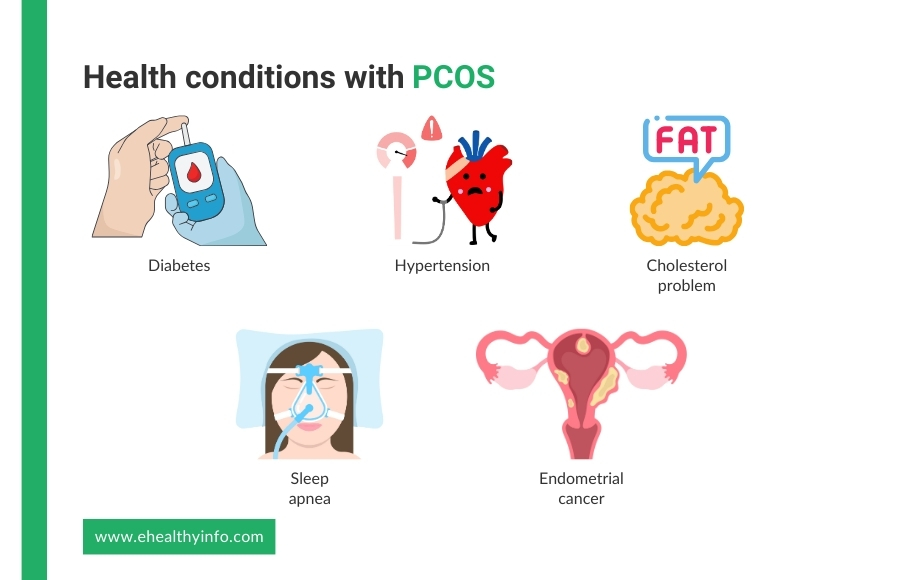
Insulin resistance is common among numerous PCOS-afflicted women, causing decreased sensitivity to insulin. Consequently, this condition can elevate blood sugar levels and heighten the likelihood of developing type 2 diabetes before reaching the age of 40.
Women diagnosed with polycystic ovary syndrome face a heightened likelihood of experiencing high blood pressure compared to those of similar age without the condition. High blood pressure represents a significant contributor to heart disease and stroke among women living with PCOS.
Women with PCOS often have higher LDL (bad) cholesterol and low HDL (good) cholesterol levels. High cholesterol also raises your risk of heart disease and stroke.
Many women with polycystic ovary syndrome are overweight or obese, which can cause repeated momentary stops in breathing while sleeping. It raises your risk of heart disease and diabetes.
Women with PCOS have been found to have an increased risk of developing endometrium cancer (lining of the uterus or womb) due to problems with ovulation, obesity, insulin resistance, and diabetes.
A single test cannot specifically diagnose PCOS. Your doctor might recommend the following to establish the diagnosis:
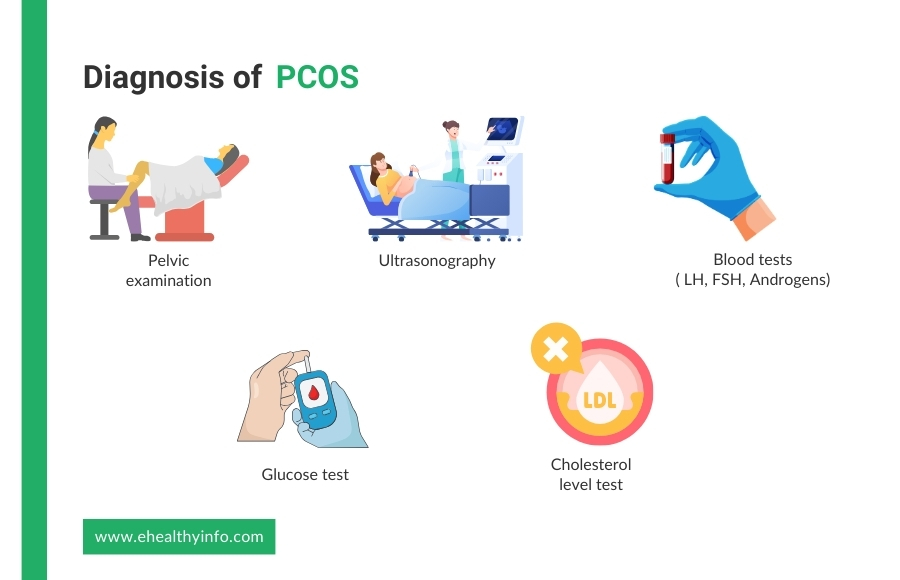
This involves a physical examination of the reproductive organs to identify abnormalities and rule out other conditions. During this exam, a healthcare provider checks for enlarged ovaries and signs of other gynecological issues, such as ovarian tumors or endometriosis.
Transvaginal ultrasound is the most reliable method for detecting polycystic ovaries. It involves placing a probe into the vagina to obtain a detailed image of the ovaries and uterus. It also helps to count the number of follicles present in the ovary. The presence of 12 or more small follicles (2-9 mm in diameter) in each ovary or increased ovarian volume (>10 mL) is a key indicator of PCOS. In the case of young or sexually inactive women, transabdominal ultrasound can be used to look for polycystic ovaries.
A blood test is used to measure the level of hormones, and it can help exclude the possible causes of menstrual problems or androgen excess that mimics polycystic ovary syndrome. The hormones that are measured are:
Other tests include tests to look for glucose intolerance, cholesterol, and triglyceride levels and screening for depression, anxiety, and sleep apnea.
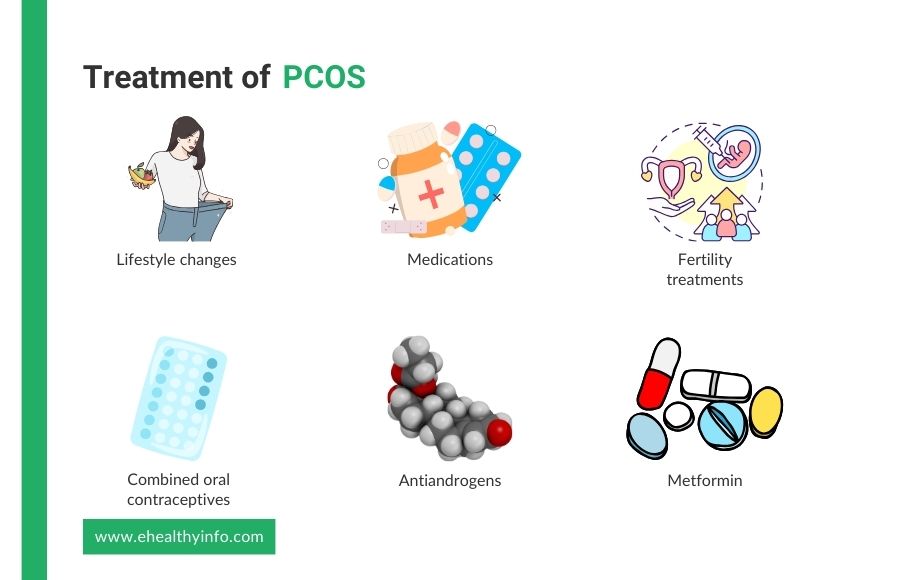
There is no cure for polycystic ovary syndrome. Treating PCOS involves addressing its diverse symptoms and underlying metabolic issues. Here are the polycystic ovary syndrome treatment options:
Weight loss is one of the most essential factors in managing PCOS. Dietary modifications with balanced nutrition and low glycemic index foods can help manage weight and improve insulin sensitivity. Regular physician activity and combining aerobic and resistance training can also help with weight reduction and reduce the risk of cardiovascular disease.
There are various medications prescribed for PCOS, and here is the list.
Polycystic ovary syndrome significantly affects pregnancy due to its impact on hormonal balance and ovulation. Women with PCOS often experience irregular menstrual cycles and anovulation, making it more difficult to conceive. The condition heightens the risk of various complications during pregnancy, including gestational diabetes, characterized by high blood sugar levels during pregnancy, which can affect both the mother and the baby’s health. Additionally, women with PCOS face an elevated risk of preterm birth, delivering before completing 37 weeks of pregnancy, which can increase the likelihood of health issues for the newborn. Preeclampsia, a condition characterized by high blood pressure and signs of organ damage, is also more prevalent in women with PCOS during pregnancy, posing serious risks to both maternal and fetal well-being. Furthermore, miscarriage rates are higher among women with polycystic ovary syndrome compared to those without the condition, adding emotional distress to an already challenging journey.
Yes, You can. Some women with polycystic ovary syndrome become pregnant without any medical intervention. However, if you are unable to get pregnant, there are treatments to enhance your fertility. Clomiphene Citrate and Letrozole are commonly used medications to induce ovulation, while Metformin can improve insulin sensitivity and menstrual regularity. When these medical treatments fail, assisted reproductive technologies, such as intrauterine insemination (IUI) and in vitro fertilization (IVF), can also be used. With appropriate medical care and support, many women with PCOS can achieve successful pregnancies.
The hormonal imbalance in POCS does not change with age, so you may continue to have symptoms of PCOS. However, in some women, the menstrual cycle gets more regular as they get closer to menopause. Moreover, the risk of health problems linked with PCOS, such as diabetes, stroke, and heart attack, increases with age. Hence, these risks may be higher in women with polycystic ovary syndrome than those without.
Weight loss is a crucial aspect of managing polycystic ovary syndrome, as it can significantly improve symptoms and overall health outcomes. Even a 5-10% weight loss can enhance insulin sensitivity, lower androgen levels, and restore regular menstrual cycles, thereby improving fertility. Weight loss also helps to reduce the risk of type 2 diabetes and cardiovascular disease. Additionally, weight loss was associated with reductions in androgen levels, which are often elevated in women with PCOS and contribute to symptoms such as hirsutism (excessive hair growth) and acne. By adopting sustainable lifestyle changes, women with PCOS can achieve healthier weight, leading to better management of the condition.