Sarcoidosis Key Highlights
- Sarcoidosis is a multisystem disorder affecting various organs beyond the lungs, such as the skin, eyes, heart, and nervous system.
- The characteristic finding of sarcoidosis is the formation of granulomas in the affected tissue, leading to inflammation and damage to the organ involved.
- Some people may not have any symptoms or have variable presentation.
- Managing sarcoidosis requires balancing medication benefits with potential side effects, often involving corticosteroids and other immune-suppressants.
- Regular monitoring and follow-ups are vital for adjusting treatments, managing symptoms, and addressing complications for a better quality of life.
Sarcoidosis
Sarcoidosis is a rare, multisystem inflammatory disease that can affect any organ in the body. It is characterized by the formation of small, abnormal clusters of cells called granulomas. These granulomas can accumulate in various tissues and organs, disrupting their normal function. Sarcoidosis most commonly affects the lungs and lymph nodes but can also involve the skin, eyes, liver, heart, and other organs.
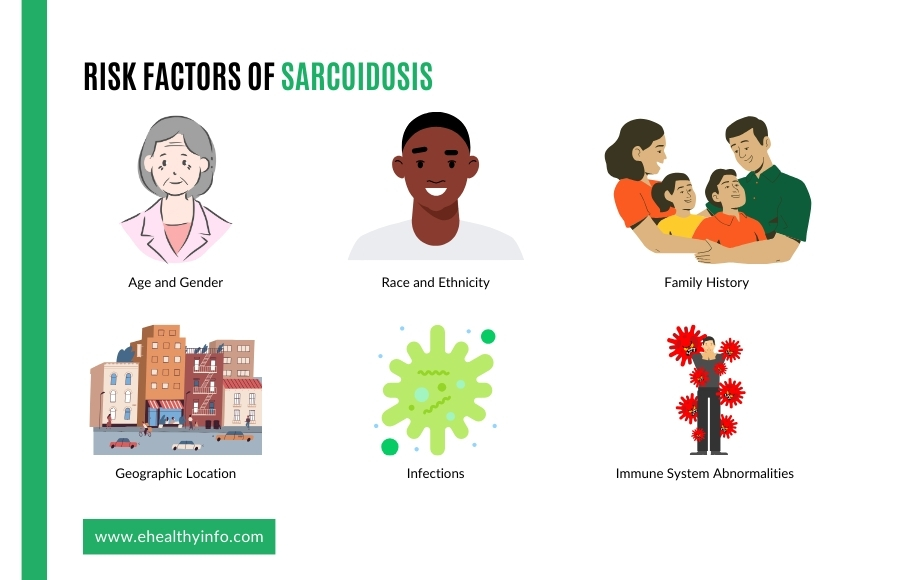
Risk Factors of Sarcoidosis
- Age and Gender: Sarcoidosis can occur at any age but often develops between 20 and 40. Additionally, it is more common in women than in men.
- Race and Ethnicity: Sarcoidosis is more prevalent in certain racial and ethnic groups, particularly African Americans and people of Northern European descent. It is less common in Asians and Hispanics.
- Family History: Sarcoidosis appears to have a genetic component, as it can sometimes run in families. If you have a close relative with the condition, it may increase your risk.
- Geographic Location: Sarcoidosis is more common in some geographic regions than others. It tends to be more prevalent in urban areas and regions with higher pollution levels.
- Infections: While not a direct risk factor, some researchers have explored the possibility that certain infections could trigger sarcoidosis or exacerbate the condition in susceptible individuals. However, no specific infectious agent has been consistently linked to the disease.
- Immune System Abnormalities: Sarcoidosis is believed to be an autoimmune disorder, meaning that the body’s immune system may mistakenly attack its tissues. People with other autoimmune conditions, such as rheumatoid arthritis or lupus, may have a slightly higher risk of developing sarcoidosis.
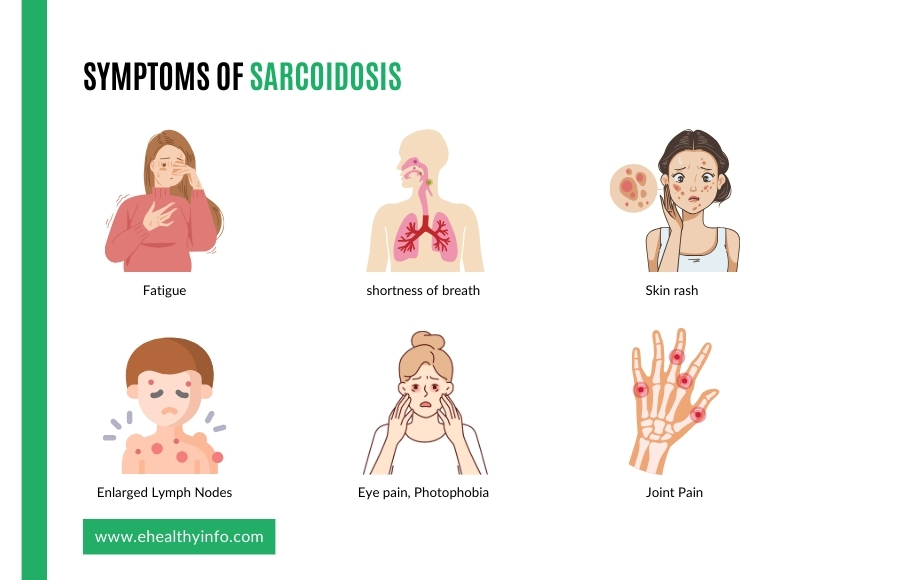
Symptoms of Sarcoidosis
Sarcoidosis can affect various organs in the body, and its symptoms can vary widely from person to person. Some individuals with sarcoidosis may have no symptoms, while others may experience various symptoms. Common symptoms of sarcoidosis include:
- Fatigue: Many people with sarcoidosis experience persistent fatigue, which can be debilitating.
- Respiratory Symptoms: Sarcoidosis often affects the lungs, leading to symptoms such as shortness of breath, cough, and even chest pain.
- Skin Symptoms: You may develop red or raised nodules on the skin that are often painful.
- Eye Symptoms: Sarcoidosis can affect the eyes, causing redness, dryness, blurred vision, and sensitivity to light.
- Joint Pain: People with sarcoidosis also complain of joint pain like arthritis. Many of them also complain of back pain and inability to bend on their waist.
- Enlarged Lymph Nodes: You may also notice swollen lymph nodes, especially in the neck, armpits, or groin.
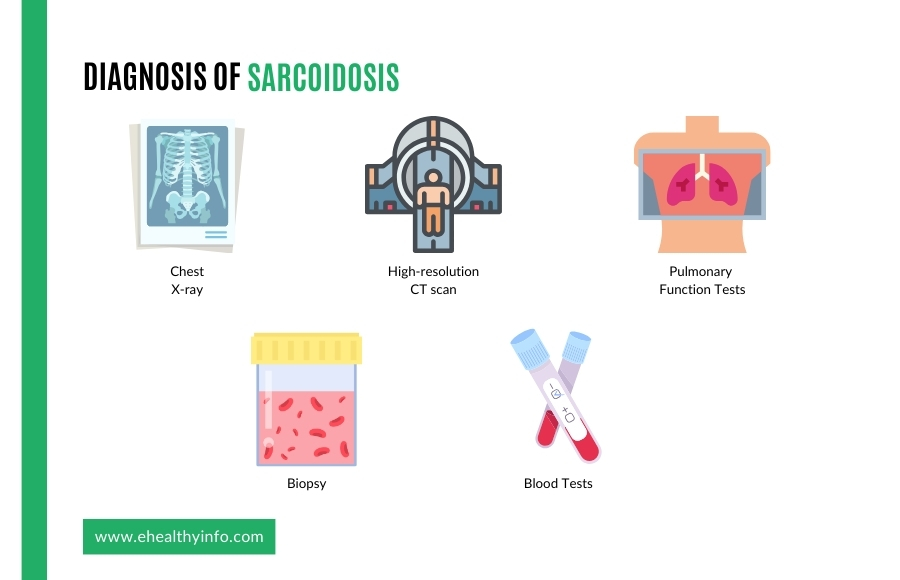
Diagnosis of Sarcoidosis
Diagnosing Sarcoidosis can be challenging because it can mimic other diseases, and there is no definitive test. It involves a combination of clinical evaluation, medical history assessment, and various tests and procedures. Here are some of the most essential tests that are done:
Imaging Studies:
- Chest X-ray: Chest X-rays are often the initial imaging tool for diagnosing sarcoidosis, primarily to assess lung involvement. In sarcoidosis, a characteristic finding on chest X-ray is “bilateral hilar lymphadenopathy,” which appears as enlarged lymph nodes in the central part of the chest. Additionally, X-rays may reveal patterns of lung infiltrates known as “pulmonary opacities,” indicating areas where the lung tissue is affected by inflammation. While X-rays can suggest the presence of sarcoidosis, they might not definitively confirm the diagnosis.
- High-resolution CT scan (HRCT): CT scans play a pivotal role in diagnosing and evaluating sarcoidosis by providing detailed images of the chest, aiding in identifying lung abnormalities, and assessing disease severity. They offer higher sensitivity than X-rays in detecting and characterizing lung involvement, showcasing features like nodules, ground-glass opacities, and fibrosis. CT scans help visualize the disease’s extent and distribution within the lungs and surrounding structures, aiding in treatment planning and monitoring disease progression. Additionally, they can identify extrapulmonary manifestations of sarcoidosis in organs like the liver, spleen, and lymph nodes, contributing to a comprehensive assessment of the disease’s systemic impact. However, while CT scans provide valuable information, they might not always definitively distinguish sarcoidosis from other lung diseases.
- Pulmonary Function Tests (PFTs): PFTs are instrumental in assessing lung function and detecting abnormalities associated with sarcoidosis. These tests measure various aspects of lung capacity, airflow, and gas exchange, providing valuable insights into the extent of lung involvement and the severity of respiratory impairment caused by sarcoidosis. In sarcoidosis, PFTs might reveal restrictive patterns characterized by decreased lung volumes due to impaired expansion and reduced gas exchange efficiency. These findings aid in monitoring disease progression, evaluating treatment response, and determining the need for interventions like medications or oxygen therapy.
Biopsy:
Biopsy is often considered the gold standard for diagnosing sarcoidosis as it allows for direct examination of tissue samples. In sarcoidosis, the characteristic finding in a biopsy is the presence of granulomas—small collections of inflammatory cells. Biopsies can be obtained from various affected organs, commonly the lungs, skin, lymph nodes, or, less frequently, from the liver, eyes, or other tissues.
Depending on the affected site, biopsies can be obtained through procedures such as bronchoscopy, skin biopsy, lymph node biopsy, or other targeted methods.
Identifying granulomas in the biopsy, along with clinical and imaging findings, is crucial for confirming a diagnosis of sarcoidosis and differentiating it from other conditions with similar presentations.
Blood Tests:
Blood tests are supportive tools in diagnosing sarcoidosis, although they do not provide a definitive diagnosis. These tests help assess inflammatory markers, immune system activity, and organ function. Standard blood tests for sarcoidosis include measurements of inflammatory markers like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which can indicate the presence and severity of inflammation. Additionally, serum calcium levels might be elevated due to granulomas’ abnormal metabolism of vitamin D. Other tests assess organ function and involvement, such as liver function tests, kidney function tests, and serum angiotensin-converting enzyme (ACE) levels, which can be elevated in sarcoidosis but are not specific to the disease.
Other Tests:
Other tests, such as eye examinations, cardiac evaluations, or nerve function tests, may be performed depending on the clinical presentation and suspected organ involvement. Sarcoidosis is a diagnosis of exclusion. Other conditions with similar symptoms and findings must be ruled out before labeling someone with sarcoidosis. Such common conditions include infections, autoimmune diseases, and other granulomatous disorders.
Treatment and Management of Sarcoidosis:
The treatment of sarcoidosis depends on the severity of the disease, the organs affected, and the individual patient’s symptoms and overall health. Treatment is aimed at reducing inflammation and managing symptoms. Here are some standard treatment options:
- Observation and Monitoring: In mild cases of sarcoidosis that do not affect vital organs and do not cause significant symptoms, doctors may recommend a “watchful waiting” approach. This involves regular check-ups and monitoring of signs and organ function to see if the disease improves.
- Corticosteroids: Corticosteroids, such as prednisone, are often the first-line treatment for moderate to severe sarcoidosis. They work by reducing inflammation and suppressing the immune system’s response. The dosage and duration of corticosteroid therapy depend on the severity of the disease and individual response.
- Immunosuppressive Medications: In cases where corticosteroids are ineffective or cannot be tolerated due to side effects, other immunosuppressive medications may be prescribed. These include methotrexate, azathioprine, and mycophenolate mofetil. These drugs suppress the immune system and help reduce inflammation.
- Biologics: In some cases, mainly when other treatments have not been successful or when there is severe involvement of specific organs, biologic agents such as tumor necrosis factor (TNF) inhibitors (e.g., infliximab, adalimumab) may be considered.
Complications of Sarcoidosis
Sarcoidosis can affect multiple organs in the body and lead to various complications. The severity and type of complications can vary significantly from person to person. Here are some of the potential complications associated with sarcoidosis:
- Pulmonary Fibrosis: The development of nodules or granulomas in the lungs can lead to lung scarring and impair lung function. Scar tissue in the lungs can cause difficulty breathing and reduced lung function. As the disease progresses, you might need a lung transplant as well.
Hypercalcemia: Sarcoidosis can cause the release of excess calcium into the bloodstream, leading to hypercalcemia, which can affect various organ systems and cause symptoms like fatigue, kidney stones, and confusion.
- Uveitis: Sarcoidosis can cause inflammation of the uvea, the middle layer of the eye. Apart from causing redness and pain, it can lead to impaired vision. This ongoing inflammation can also increase the pressure on the eye, further contributing to vision impairment.
- Cardiac sarcoidosis: Sarcoidosis can affect the heart, leading to arrhythmias, heart block, and heart failure. Cardiac involvement can be life-threatening.
- Neurological Involvement: In rare cases, sarcoidosis can affect the nervous system, causing symptoms such as headaches, facial weakness, seizures, and cognitive changes.
Questions for your doctor
- What are the potential triggers that might have caused sarcoidosis?
- What treatment options are available, and which is recommended for my situation?
- Are there any possible side effects or risks associated with the prescribed treatment?
- How long is the treatment expected to continue, and what are the desired outcomes?
- What lifestyle changes or precautions should be taken to manage sarcoidosis effectively?
- What should be the frequency of follow-up appointments and tests to monitor the condition’s progress?