Mr. Watkins is a 55-year-old war veteran. He recently lost his job and is divorced from his wife. He has been drinking more lately and has recently started using cocaine occasionally too. He told his friend that he no longer saw reason to live, and thoughts of shooting himself have been cropping up in his mind. What can his friend do to help?
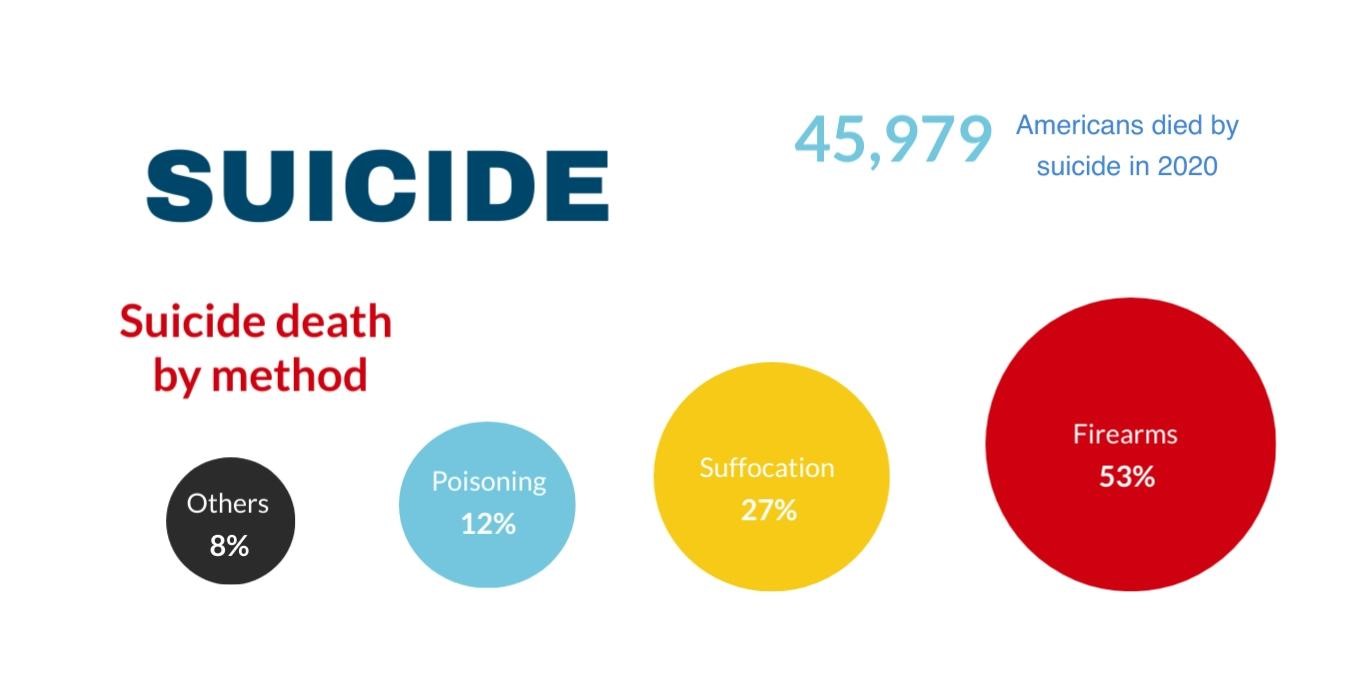
Suicide is the act of killing oneself or harming oneself to the point of death. In the United States alone, CDC reports one death by suicide every 11 minutes. Common methods of suicide are firearms, suffocation, and overdose or poisoning.
In our usual state of mind, it does not make sense why anyone would choose death over life, leaving their family, friends, and loved ones alone and devastated. When someone is under extreme distress from mental health issues or other stressors, it might feel like taking one’s own life is the only way to end the misery. For others, suicidal thoughts might look sudden and come out of nowhere. Usually, thoughts of suicidal thoughts grow gradually over time, and people express those thoughts to others before they act on them. They tend to be ambivalent about it and anything we can do to delay or limit immediate access to tools people use for suicide can save a life.
We are not comfortable talking about suicidal thoughts. It is tough to talk with people close to us as they fear how it might affect others or how they will react. We can detect suicidal thoughts by talking to them, especially by listening to them. Asking others about suicidal thoughts does not increase the chances of having suicidal ideation, contrary to what many people still believe.
The stigma associated with mental health warrants more initiative and activities to increase awareness in the community. On the one hand, there are not enough trained mental health professionals; on the other hand, people hesitate to use available resources. Hence, recognizing those at risk for suicide, providing support, and assisting them in getting resources are crucial to lowering someone’s risk of suicide and improving their mental health.

People with suicidal thoughts or someone who has attempted suicide may not always look sad or any different than usual. As suicidal ideations get stronger, they might feel like all other doors are closing around them and start believing dying is the only option left. There is no definite way to predict who will or will not attempt to take their own’s life. However, some factors that increase the risk of future suicide are as follows;

Many people who take their own’s life may not show any signs, but they may leave some clues based on their behavior. The more warning signs a person exhibits, the greater the risk of suicide. The following behaviors are some of the warning signs of suicidality.

We must listen to the individual without judgment. Someone talking to you about killing themselves is an emergency and needs immediate attention. Someone responsible and trusted has to accompany the person at all times.
Getting rid of objects that cause harm, fatal or otherwise, does make a difference. If someone has access to firearms, it is essential to take them away. While this is not always easy, ask if they have any plans to carry out a suicide attempt.
Those at immediate risk of hurting or killing themselves should be taken to the hospital immediately. It is best to call 911 for EMS support if they are in immediate danger to themselves and it is unsafe to transport them to ED by other means.
The suicide prevention telephone line or crisis center can be contacted if your friends, family, or anyone else shows signs of suicidal behavior. The program is a federally funded service and is free, available to anyone, and is open 24 hours a day, every day of the week. You can always dial National Suicide Prevention Lifeline (1-800-273-TALK (8255)) or the Crisis Text Line’s number (741741) from your phone. All calls are confidential. Staying in contact and supporting the person after the suicide crisis is very important and shows you care about the person.
It is essential people with suicidal thoughts get help from a licensed mental health professional. You can assist patients in finding or helping them start service with a trained mental health professional.

A suicide crisis is when someone is attempting to kill themselves or seriously thinking of doing so. Mental health professionals are trained to do a thorough risk assessment of anyone seeking their help and treatment of underlying mental health disorders. Mental health experts work with patients to find the best treatment option, including a medication regimen, to help overcome their crisis and treat any other mental health problems the patient may have. Different treatment modalities, including but not limited to psychotherapy, medications, and safety planning, help overcome the suicide crisis and prevent future suicide attempts. One of the most important parts of safety planning is limiting access to lethal means to harm oneself, such as firearms, pills, or poison. Talk therapy can help people learn about illness and new ways of dealing with stressful situations. Talk therapy helps people who have attempted to take their own’s life recognize their thought patterns and consider alternative actions when they have suicidal thoughts to prevent them from carrying out suicide in the future.
Most mental health problems are chronic and need follow-up services and continued support in the community.
Call 911 if you or someone you know is in immediate danger, or go to the nearest emergency room.
National Suicide Prevention Lifeline
Call 1-800-273-TALK (8255); En español 1-888-628-9454
Use Lifeline Chat on the web.
Crisis Text Line
Text “HELLO” to 741741
Veterans Crisis Line
Call 1-800-273-TALK (8255) and press 1 or text to 838255
Use Veterans Crisis Chat on the web
Disaster Distress Helpline
Call or text 1-800-985-5990