
A Urinary Tract Infection (UTI) occurs when bacteria enter the urinary system, which includes the kidneys, bladder, ureters, and urethra. It commonly causes symptoms like a burning sensation when you urinate, the need to urinate frequently, and cloudy or strong-smelling urine.
UTIs can affect men and women of all age groups. However, the incidence is higher in females. About 50% of women report having UTIs at some point in their lives. [1]
There are various ways to classify UTI depending on various factors. On the basis of the onset of symptoms, it can be:
Based on whether the infection is complicated or not, there are two types of UTIs, namely,
This is usually less serious. A case of UTI is considered uncomplicated when there is no structural or functional abnormality of the urinary tract, and there are no significant comorbidities.[3]
UTI is classified as complicated under specific circumstances. These include if the patient is a child or pregnant, if there are structural or functional abnormalities in the urinary tract if the patient has underlying comorbidities such as diabetes, or if there has been recent instrumentation or surgery involving the urinary tract.[3]
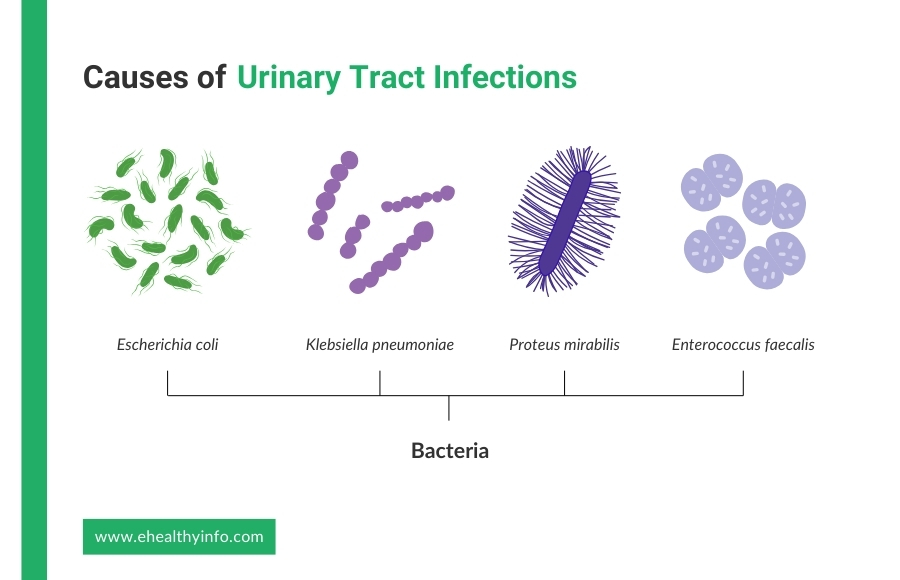
UTIs are primarily caused by bacteria, with Escherichia coli (E. coli) being the predominant pathogen. E.coli accounts for 70-95% of community-acquired UTIs.[4] Other common causative agents include Klebsiella pneumoniae, Proteus mirabilis, and Enterococcus faecalis. [4]
The most typical way these pathogens infect the urinary tract is through the ascending route, where bacteria travel from the urethra up to the bladder and potentially to the ureters and kidneys. They first colonize the areas around the urethra and then move upward. Less commonly, infections can spread through the bloodstream (hematogenous route) or lymphatic system. [5]
Several host factors increase the risk of UTIs, such as being female, pregnancy, frequent or recent sexual activity, difficulties in urinating, and the use of spermicides. Recent antibiotic use and conditions like vesicoureteral reflux also elevate the risk. [2]
UTIs present with various signs and symptoms, which vary depending on the location and severity of the infection. The primary symptoms include:
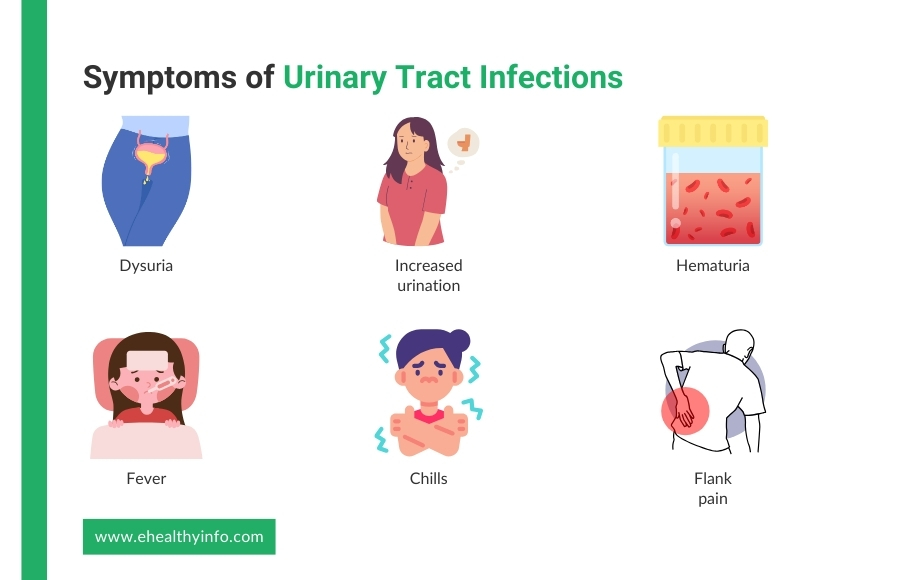
This is a burning sensation you have during urination. This symptom indicates inflammation or irritation in the urethra or bladder.[6]
Many people experience an increased need to urinate, often producing only small amounts of urine each time. This symptom suggests bladder involvement.
Blood in the urine is a common symptom. It can range from microscopic hematuria, detectable only through a urine test, to gross hematuria, where blood is visible in the urine.[7]
In cases where the infection ascends to the kidneys (called as pyelonephritis), you might experience symptoms such as fever and chills.[8]
Pain in the back or side, below the ribs, can indicate a kidney infection. This symptom is often severe and requires immediate medical attention. You may also experience nausea and vomiting. [9]
Your symptoms can easily suggest a UTI, and your doctor can order other tests to confirm the diagnosis. Here are some of the tests that you might require:
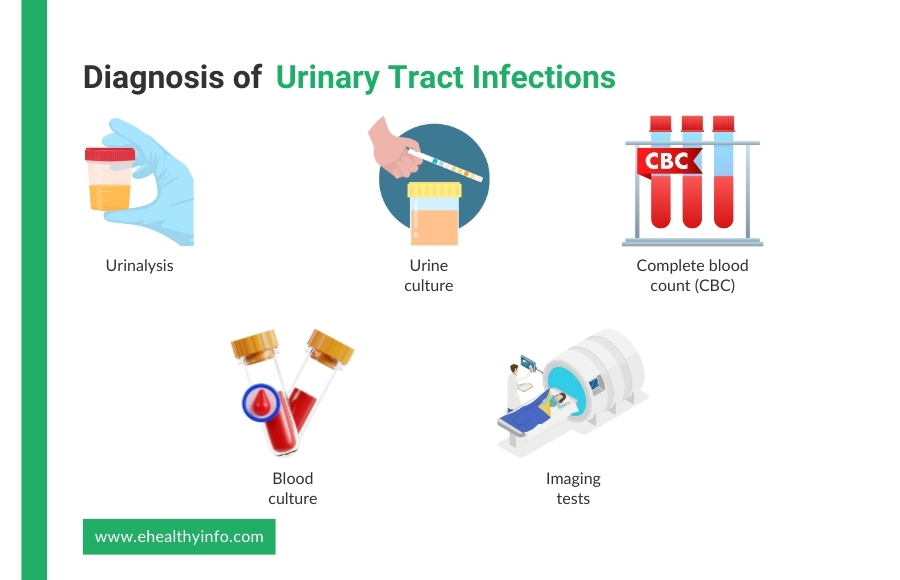
This is the first step in diagnosing a UTI. A sample of urine is analyzed for the presence of white blood cells, red blood cells, and bacteria. The presence of nitrites and leukocyte esterase in the urine is a strong indicator of a UTI.[10]
To confirm the diagnosis and identify the specific bacteria causing the infection, your doctor can ask for a urine culture. The sample is incubated to allow any bacteria present to grow. This test can also determine the sensitivity of the bacteria to various antibiotics, guiding effective treatment.[11]
A CBC can help identify the presence of an infection by showing elevated white blood cell counts, which is a sign of the body fighting off an infection. This is primarily done when you are suspected to have a kidney infection, as this can further help to figure out if your infection has subsided or not after the antibiotic therapy. [12]
In severe cases, especially when a kidney infection is suspected, blood cultures may also be taken to check if the infection has spread to the bloodstream.[12]
While not typically part of the initial laboratory diagnosis, imaging tests such as an ultrasound, cystoscopy, computed tomography scan, or magnetic resonance imaging can be used if there are concerns about structural abnormalities or complications like kidney stones or abscesses that might be responsible for your UTI. These tests may also be performed if you have recurrent UTIs. [13]
Urinary tract infections can lead to a range of complications if not treated promptly and adequately. Some of such complications are:
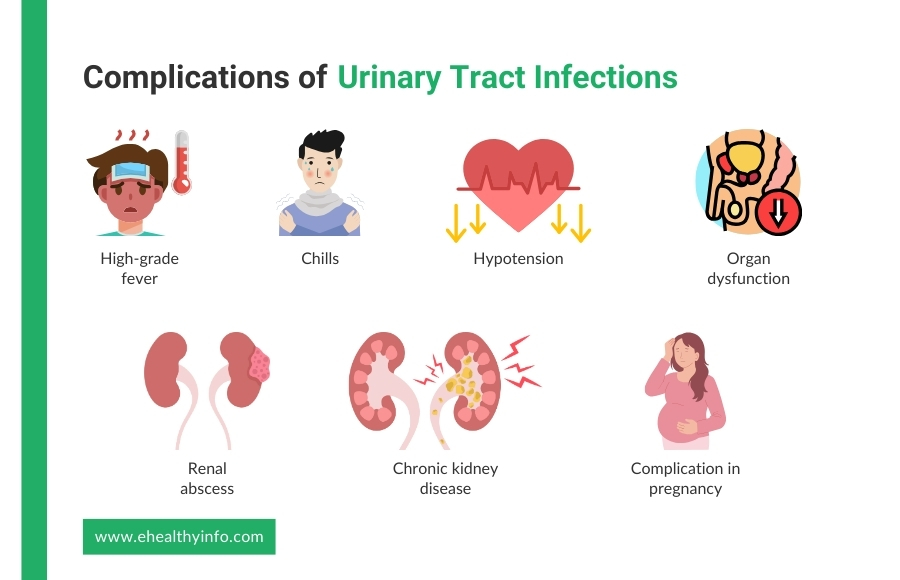
It is a severe systemic response to a UTI that spreads to the bloodstream, leading to sepsis. High-grade fever, chills, hypotension, and organ dysfunction are the symptoms.[14]
An improperly treated UTI, especially pyelonephritis, can result in the formation of a renal abscess. Renal abscess is a localized collection of pus within the kidney tissue.[8]
Recurrent or severe UTI can cause permanent renal damage and scarring. Over time, this leads to chronic kidney disease, reducing kidney function.[15]
UTIs in pregnancy increase the risk of complications such as preterm labor and low birth weight.[16]
The treatment options for urinary tract infections vary depending on the type and severity of the infection. They encompass both pharmacological and non-pharmacological approaches.
The mainstay of treatment for UTI is antibiotic therapy. The first-line antibiotics often include trimethoprim-sulfamethoxazole, nitrofurantoin, and fosfomycin. These antibiotics are chosen for their effectiveness against common UTI pathogens. In cases where there is resistance or recurrent infections, culture-specific antibiotics are prescribed based on the sensitivity profile. The duration of treatment typically ranges from 3 to 7 days for uncomplicated UTIs and a longer duration of about seven to fourteen days for complicated ones to ensure complete eradication of the infection. [9]
To alleviate urinary discomfort, analgesics such as phenazopyridine can be used. This medication specifically targets urinary tract pain. Meanwhile, over-the-counter pain relievers like ibuprofen or acetaminophen can be used to manage general discomfort and reduce inflammation associated with the infection.[10]
Drink plenty of fluids, as they are important for flushing bacteria from the urinary tract. Water is the best choice for hydration.[17]
Preventive measures for urinary tract infections are important, particularly for individuals prone to recurrent infections. Here are five preventive measures you can follow:
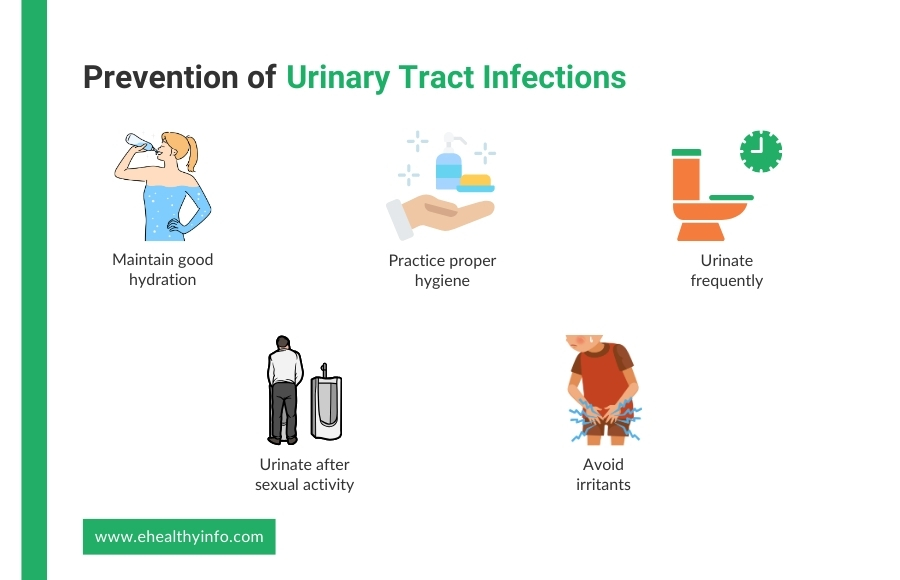
Drink plenty of fluids, especially water, to help flush bacteria from the urinary tract.[17]
Wipe from front to back after using the toilet to prevent bacteria from the anal area from spreading to the urinary tract.[18]
Do not hold urine for long periods. Emptying the bladder regularly can help prevent bacterial growth.[19]
Urinating after intercourse can help flush out bacteria that may have entered the urinary tract.[19]
Avoid using irritating feminine products such as deodorant sprays, douches, and powders in the genital area. These can cause irritation and increase the risk of infection.[19]
Prophylactic antibiotic therapy is particularly important in those with recurrent urinary tract infections. Your doctor will prescribe antibiotics for daily use at a dose lower than required to treat the infection, which helps to reduce the frequency and severity of episodes.
The antibiotics are the same as the ones used for treatment but at a lower dose, and the choice depends on the local antimicrobial resistance pattern.[20]
Cranberry juice has long been suggested as a natural remedy for preventing UTIs. The primary mechanism behind this is the presence of proanthocyanidins in cranberries, which are believed to prevent bacteria, particularly E. coli, from adhering to the walls of the urinary tract. By inhibiting bacterial adhesion, cranberry juice may help reduce the likelihood of a developing infection. [21]
However, while some studies support the potential benefits of cranberry juice in preventing UTIs, the evidence is not conclusive. It’s important to note that cranberry juice should not replace standard medical treatments and prevention strategies for UTIs. Those considering using cranberry juice as a preventive measure should consult with their doctor, especially if they have recurrent UTIs or other underlying health conditions.[21]