
Colon Cancer
Colon cancer, also known as colorectal cancer, is one of the most common forms of cancer. It originates in the colon or rectum, often as a growth called a polyp. Over time, these polyps can become cancerous, making it crucial to detect and treat them early. This cancer can be highly aggressive, spreading to other parts of the body if not diagnosed and treated in its early stages. Colorectal cancer (CRC) is the third most common cause of death for both men and women. It is most frequently diagnosed among persons aged 65 to 74, and approximately 10.5% of new colorectal cancer cases occur in people under 50.
The exact cause of colon cancer is not fully understood, but certain risk factors can increase your likelihood of developing the disease. They are discussed below:
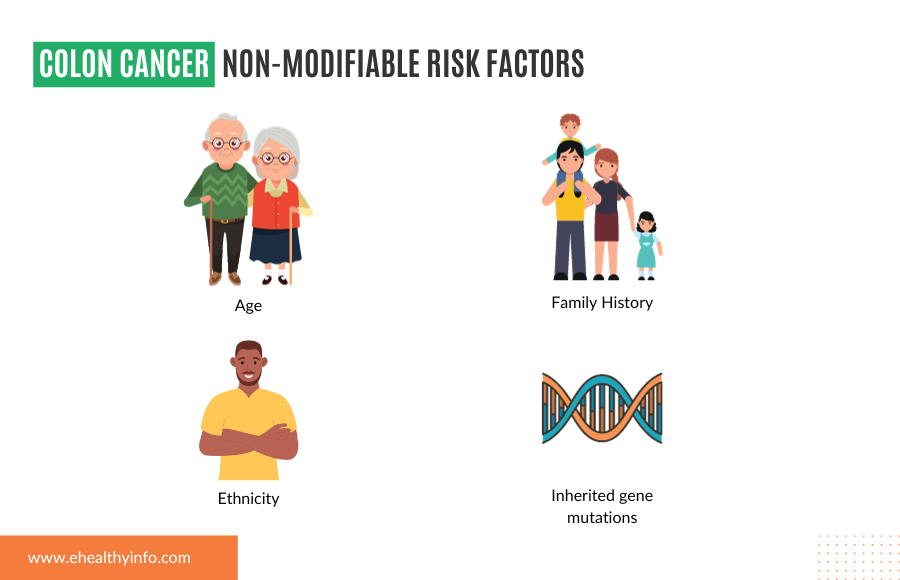
Non-modifiable risk factors of colon cancer:
These are the risk factors you do not have control over. They are factors that you are born with, and you cannot do anything to modify them to decrease the risk.
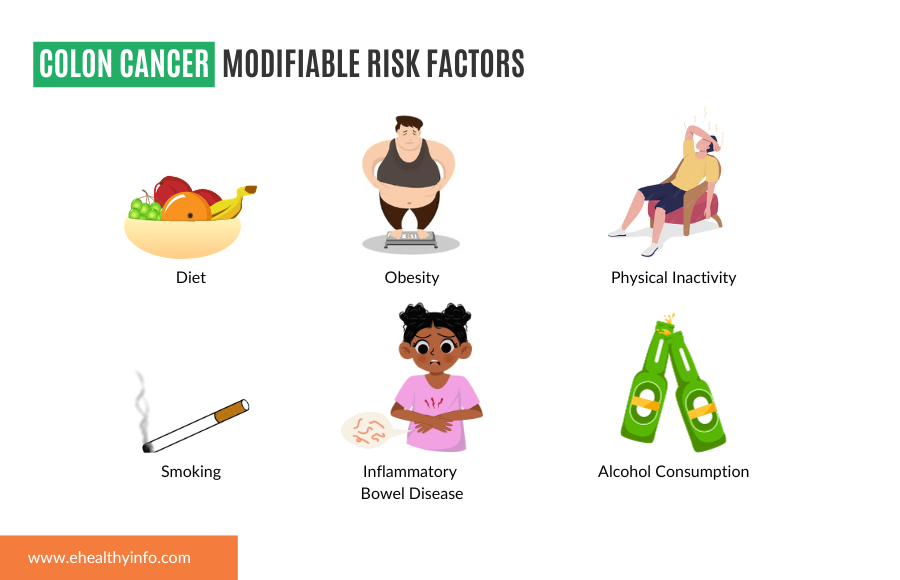
Modifiable risk factors of colon cancer:
These are risk factors that you can modify through behavioral, medical, or environmental interventions. Some of the modifiable risk factors of colorectal carcinoma are:
Colorectal cancer may not present with symptoms in its early stage and can reach a point where it might be difficult to cure. It is essential to keep note of the symptoms that can help to detect these cancers in their early stage.
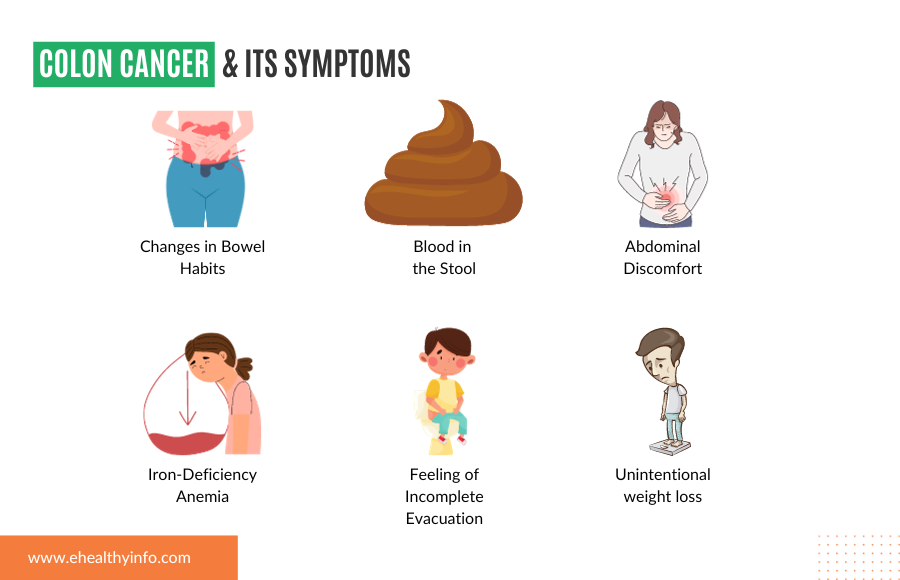
1. Changes in Bowel Habits:
2. Blood in the Stool:
3. Abdominal Discomfort: Colorectal cancer can cause cramps or aches in your lower abdomen that don’t seem to go away, even with over-the-counter remedies.
4. Unexplained Weight Loss: If you’re shedding pounds without trying, it could be due to changes in your digestive system caused by cancer.
5. Iron-Deficiency Anemia: This occurs when your body doesn’t have enough iron, often due to chronic bleeding in the colon. Symptoms may include weakness, paleness, and shortness of breath.
6. Feeling of Incomplete Evacuation: You may feel the need to have a bowel movement but can’t empty your bowels. This can be one of the signs of colon cancer.
Colorectal cancer, when caught early, is highly treatable and often curable. Screening for colorectal cancer is a proactive step that can make all the difference in the world.
Q. Who should be screened?
Screening guidelines typically recommend that individuals at average risk for colorectal cancer begin screening at age 45. However, the age at which screening should begin may vary based on individual risk factors, family history, and genetics. Those with a family history of colorectal cancer or certain genetic syndromes may need to start screening earlier.
Colon Cancer Screening Guidelines
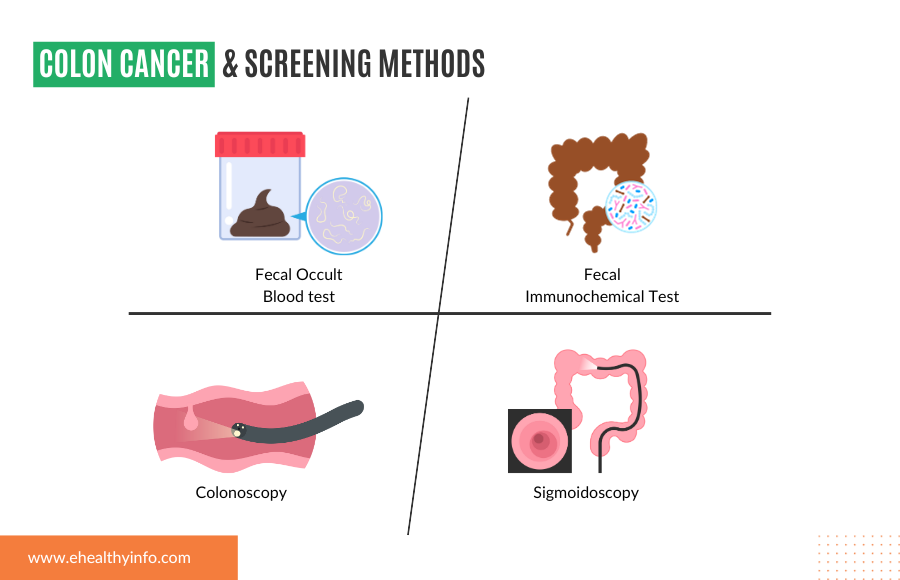
Screening methods
Screening frequency
Your doctor might employ various ways to detect and diagnose the presence of the carcinoma. Here is the list of tests that your doctor might suggest:
1. Blood tests: Blood tests play a crucial role in the detection and monitoring of various medical conditions that you have, including colorectal cancer. It is important to remember that blood markers are not diagnostic on their own and are used as a part of a comprehensive assessment. The test includes:
2. Colonoscopy and biopsy: colonoscopy is a procedure that utilizes a flexible tube with a camera that offers real-time visualization of the colon and rectum, enabling the detection of precancerous polyps and tumors. If your doctor detects abnormalities, biopsy samples can be obtained during the procedure, allowing for a definitive diagnosis by examining the tissue under a microscope. These crucial steps confirm the presence of colorectal cancer, determine its type stage, and guide treatment decisions.
3. Imaging: Various imaging techniques are employed in the context of colorectal cancer. Computed Tomography (CT) scans provide detailed cross-sectional images of the abdomen and pelvis, making them useful for staging and monitoring response to treatment. Magnetic Resonance Imaging (MRI) offers high-resolution images of the pelvis, aiding in assessing the local extent of the tumor and lymph node status. Positron Emission Tomography (PET) scans detect distant metastases and assess the metabolic activity of lesions, enhancing staging accuracy when combined with CT or MRI. Ultrasound is utilized for assessing rectal tumors, providing real-time imaging during certain procedures. Not everyone requires all the tests; your doctor will suggest the right test for you.
There are various treatment options available for colorectal cancer, and they depend on numerous factors, including the location of the tumor, tumor stage, overall health, and many more.
Here is the list of treatment options available:
1. Surgery: Surgery is the most common treatment for colon cancer at all stages, which involves removing the tumor during an operation. The nature of the cancer determines the type of surgery. It can be local excision for a limited tumor or extensive resection for a cancer that has spread.
2. Radiofrequency ablation: Radiofrequency ablation (RFA) is a minimally invasive medical procedure gaining prominence in treating colorectal carcinoma, particularly for certain cases of liver metastases originating from colorectal cancer. It employs high-frequency electrical currents to generate heat, effectively “cooking” and destroying cancerous tissue. RFA can be used alone or with other treatment modalities, such as surgical resection, chemotherapy, or targeted therapies.
3. Chemotherapy: Chemotherapy is a systemic treatment strategy commonly employed in colorectal carcinoma. It utilizes drugs to target and destroy cancer cells throughout the body, making it particularly useful for advanced-stage colorectal cancer or when cancer has spread to other organs. Chemotherapy may be administered before surgery to reduce the size of tumors, post-surgery to eliminate any remaining cancer cells, or in combination with other therapies such as radiation or targeted therapies. Common chemotherapy drugs for colorectal carcinoma include 5-fluorouracil (5-FU), oxaliplatin, and irinotecan. Although chemotherapy can effectively slow cancer growth and extend survival, it may also produce side effects, such as fatigue, nausea, and lowered blood cell counts, which medical professionals closely monitor and manage.
4. Radiation therapy: High-energy X-rays or other forms of radiation are used in radiation therapy, which helps to kill or stop cancer cells’ growth. External radiation therapy uses a device outside the body to direct radiation at the cancerous region. Internal radiation therapy uses catheters, seeds, wires, or needles with radioactive materials sealed inside that are inserted into or close to the malignancy.
5. Targeted therapy: Targeted therapy is a form of medical care that isolates and destroys particular cancer cells using medicines or other substances. Compared to chemotherapy and radiation therapy, targeted therapies often don’t kill healthy cells as much.
6. Immunotherapy: Immunotherapy is a cancer treatment that activates the patient’s immune system. The body’s natural defenses against cancer are boosted, directed, or restored using substances produced by the body or in a lab. Biologic therapy is a kind of treatment for cancer.