John is a 65-year-old man. He has recently noticed swelling in his legs and gets tired more often than he used to. He gets shortness of breath more often when he goes for a short walk. His doctor thinks he could have heart failure.
Our heart acts as a pump. It fills blood while resting and empties when squeezing. The pump doesn’t work properly when it’s too weak or stiff. This failure of the heart’s pumping mechanism is called heart failure. It doesn’t mean the heart has completely “failed” or stopped working.
Heart failure can affect one or both sides of the heart. Our heart has two working parts- the left and the right. In left heart failure, the left side of the heart must work harder to pump the same amount of blood. Similarly, in right heart failure, the right side of the heart has to work harder and is under stress from pumping blood in your body. You will hear your doctor talk about two types of heart failure: systolic heart failure and diastolic heart failure.
Systolic heart failure or Heart failure with reduced ejection fraction (HFrEF): Here, the left ventricle loses its ability to contract normally. The heart can’t pump with force to push enough blood into the bloodstream.
Diastolic heart failure or Heart failure with preserved ejection fraction (HFpEF): Here, The left ventricle loses its ability to relax, and as a result, the heart can’t appropriately fill with blood during the resting period between each heartbeat.

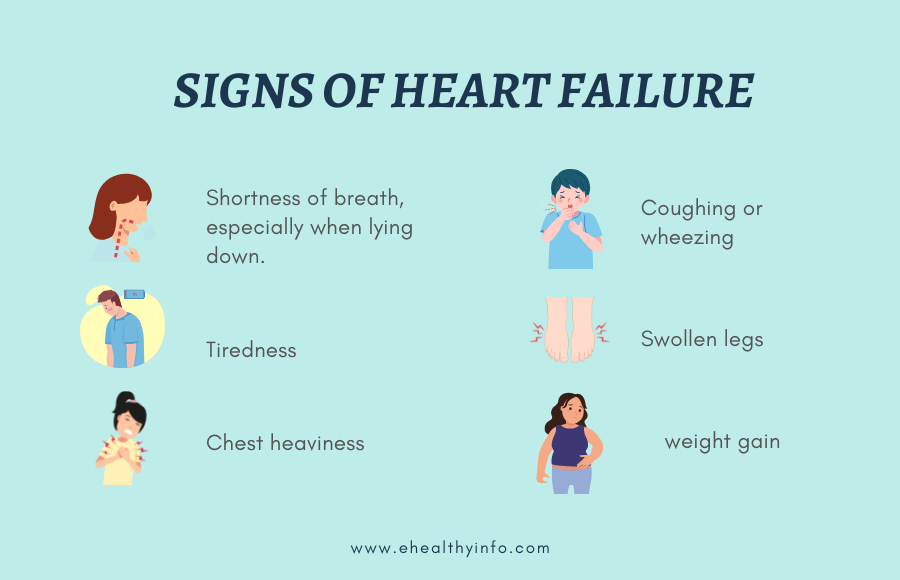
The symptoms of heart failure depend on how much your heart fails to pump blood in the body. The more your heart grows weaker, the more you may become short of breath, sometimes even when lying down. You may experience fatigue and generalized weakness when you have heart failure. For instance, you will feel short of breath after routine activities like climbing stairs or working in an office or kitchen.
Some people struggle with weight gain due to water retention and abdominal and leg swelling. The symptoms of heart failure can be very slow to show. However, you will know your heart is weakened if you have a heart attack.
Your doctor might suspect you have heart failure based on the symptoms such as swelling of the body or shortness of breath during activities that require low stamina. Most people who develop heart failure might have other underlying heart conditions too. Your doctor will ask you if you have coronary artery disease, high blood pressure, irregular heart rhythm, or a previous heart attack to ascertain if you have heart failure or are at risk.
Your doctor can order a chest x-ray, electrocardiogram (electrical tracing of the heart), and echocardiogram (ultrasound of the heart) to evaluate your heart failure. Blood tests are also available to check if there is an increased strain on the heart.
An echocardiogram is simply an ultrasound of your heart. It uses sound waves to take detailed pictures of your heart which help your doctor evaluate how much your heart is pumping blood and if it is functioning correctly.
What is ‘ejection fraction’?
An ejection fraction compares the amount of blood in the heart to the amount of blood pumped out. Your doctor might tell you that you have an ejection fraction (EF) in percentage. This percentage helps describe how well the heart pumps blood to the body.
What’s a normal ejection fraction?

Your primary care provider or cardiologist will need to tailor your treatment plan for heart failure depending on its cause, symptoms, and ejection fraction. Your symptoms can improve quickly after starting a treatment plan, but you must not leave your medication plan or stop seeing your doctor if this happens. You will benefit from following up with your doctor every 3 to 6 months, even if you show no symptoms. Many hospital systems and cardiologists have special heart failure clinics that will follow up with you for a long time to ensure your heart is functioning properly.
Many patients with heart failure take diuretics, also called water pills, to remove excess fluid, which helps alleviate symptoms. Many other medications have proven beneficial for patients and allow them to live longer and avoid hospitalization. The doctor must gradually introduce these medications to you so you can tolerate them. Your doctor will slowly add these medications to your treatment plan. Your doctor must ensure your blood pressure, kidney functions, and electrolytes are well maintained while heart failure medications are introduced.
Depending on your ejection fraction, your cardiologist may recommend pacemakers and implantable cardioverter-defibrillators. These devices can help strengthen your heart and prevent life-threatening abnormal heart rhythms. In very advanced heart failure, you might need an artificial heart pump (also known as a left ventricular assist device) or a heart transplant.
When you have a new diagnosis of heart failure, your doctor will evaluate you for coronary artery disease. This disease causes the narrowing of the arteries that supply blood to the heart. Evaluating the coronary arteries might involve taking more images of the heart, called a ‘stress test’ or a percutaneous coronary angiogram. In a coronary angiogram, an interventional cardiologist will introduce a catheter and use dyes to assess flow efficiency in arteries supplying blood to the heart. If the heart’s arteries are blocked or narrowed, the cardiologist can inflate the narrowed arteries with a balloon or put in a permanent stent. This specialized procedure is called Percutaneous Coronary Intervention (PCI). A stent can permanently hold your artery open, resulting in adequate blood flow to the arteries and helping prevent further narrowing of the artery. This specialized procedure is called Percutaneous Coronary Intervention (PCI).
Don’t forget to talk to your doctor regarding lifestyle changes you can make to limit the progression of your heart failure. Diet and exercise are critical to managing heart failure.
Your doctor can prescribe:
Cardiac Rehabilitation is a program for the heart that involves various activities to stop the progression of cardiovascular disease. This multidisciplinary program helps change the lifestyle of afflicted individuals and, ultimately, decreases hospital readmission and death. It is usually located in or affiliated with your hospital and can consist of 2 to 3 hours sessions per week and lasts 12 to 18 weeks. Talk to your doctor regarding Cardiac Rehabilitation.
Cardiac Rehabilitation activities can include:
Your doctor will recommend you join a Cardiac Rehabilitation Program if you have one or more of the following conditions:
Heart failure prevention involves living a healthy lifestyle and proper medical treatment for conditions predisposing one to heart failure.
Some ways to prevent heart failure are:
Other ways to manage conditions that make one more likely to have heart failure are:
Talk to your doctor about whether your heart function needs to be monitored if you have any of the above underlying conditions.

Traditionally, patients with heart failure are suggested to restrict their salt intake. Some studies have revealed no reduction of significant adverse effects and hospitalization reduction in patients who restricted their salt intake. However, there was a significant improvement in their quality of life, and progression of the heart disease was slowed down in patients who restricted salt intake. While we suggest people limit their salt intake, it is unnecessary to completely omit salt in their diets.
Heart failure treatment plans need regular monitoring at home. You can make a log book of your weight at least a few times weekly to ensure you have not gained excess water. The logbook can help your doctor decide on what dose of diuretics (water pills) to prescribe to you to help improve your symptoms and alert you about when to call your doctor.
It would be best if you tracked the following in your logbook.
Heart failure treatment involves a multidisciplinary team, and so, your participation and home monitoring are vital for you to recover. When heart failure is left untreated, your heart can weaken severely and cause life-threatening complications. You will need regular follow-ups with your doctor to control heart failure.
Heart failure can happen to anyone. Do not hesitate to contact your doctor if you suddenly have any new or unexplained symptoms that may indicate a heart problem. It is always better to be safe than sorry, after all.