
Our elderly population can be diverse, ranging from healthy, active, and healthy octogenarians to extremely frail, totally dependent people with chronic disease and severe disabilities. As people age, their body composition changes, which has an impact on their nutritional status. Malnutrition is a common problem among elderly individuals, which is defined as the state of being poorly nourished.
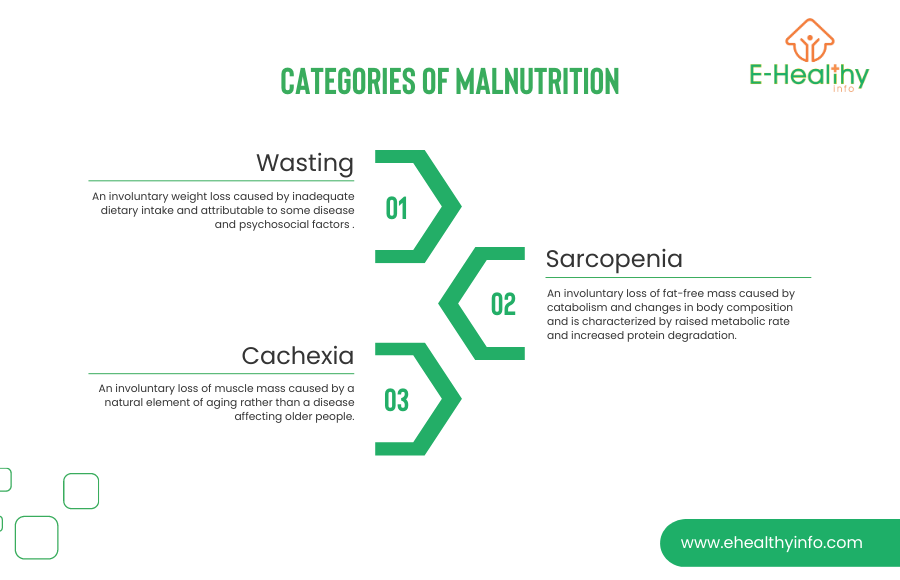
Malnutrition or poor nutrition leads to serious health problems such as anemia, osteoporosis, impaired immune function, non-healing wounds, and prolonged time to recover from illnesses. It may be caused by the lack of one or more nutrients (undernutrition) or an excess (overnutrition). Weight loss and malnourishment come in the elderly population in different forms.
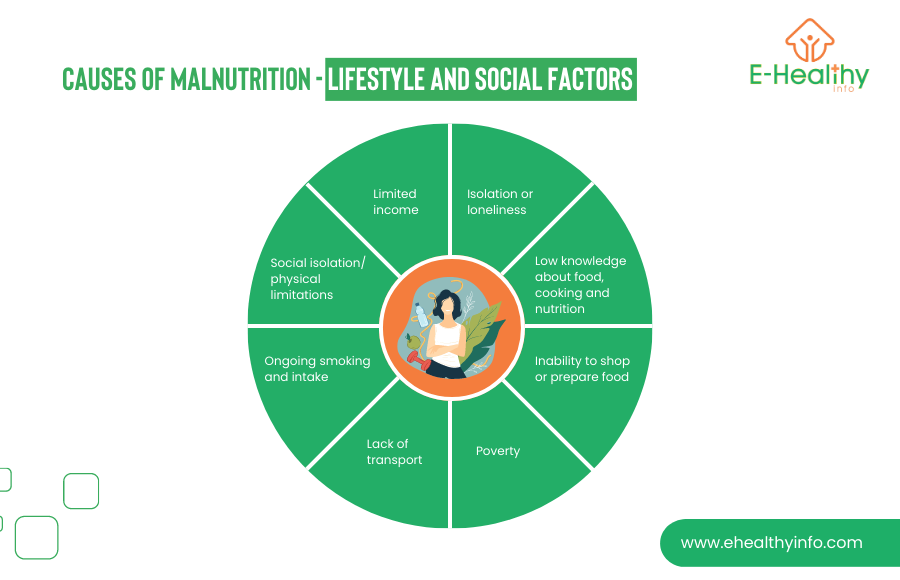
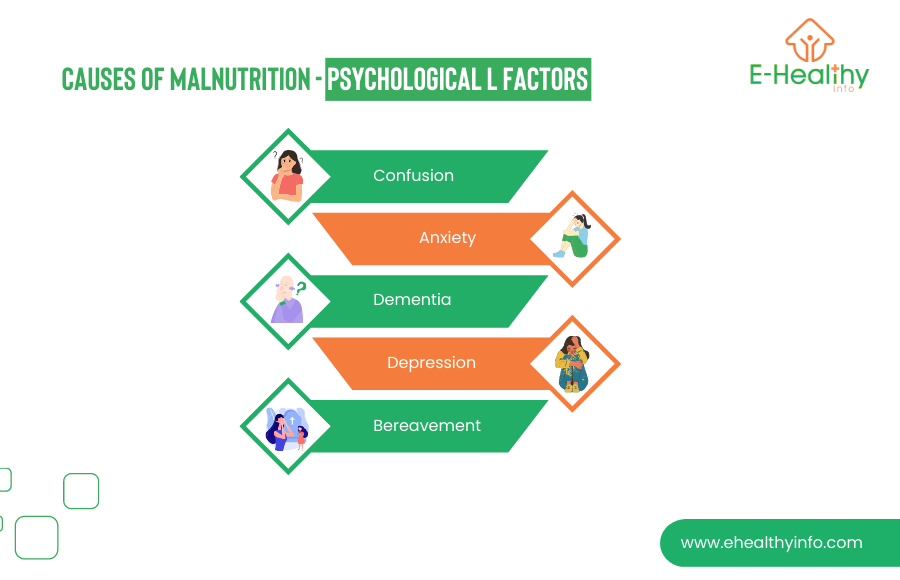
One can be at high risk for malnourishment due to multiple factors ranging from a poor appetite/ inadequate energy intake and nutrients, difficulty chewing or swallowing, and certain medications/ polypharmacy. It is easier to simplify the causes of malnutrition based on medical, lifestyle, and psychological factors.
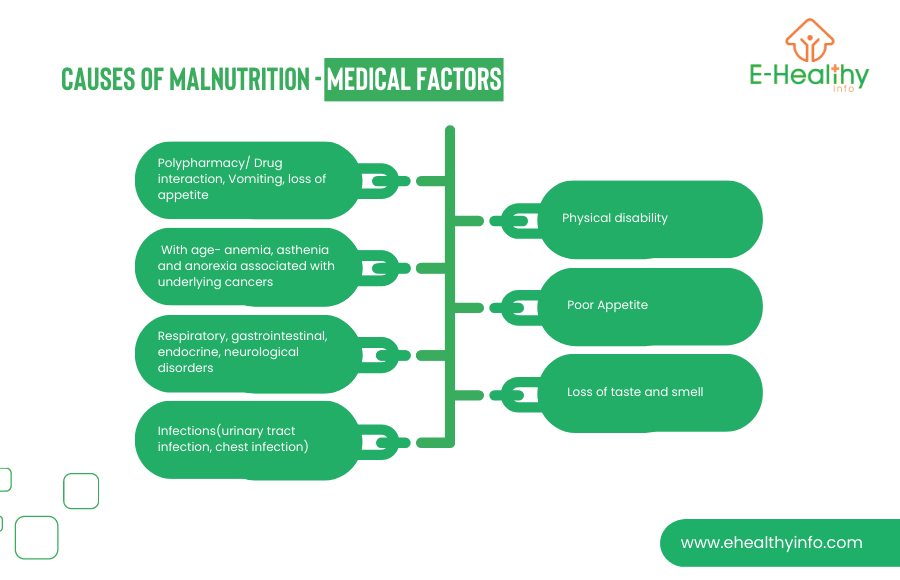
Medical factors:
Lifestyle and social factors:
Psychological factors:
There are no generally accepted criteria for diagnosing malnourishment in the elderly. Your doctor may do a quick Mini Nutritional Assessment (MNA) and Nutritional Risk Screening (NRS) to identify malnutrition in the clinic quickly. Your doctor will focus on the following points to evaluate the nutrition degree.
○ Low body weight or changes in appetite/ Significant weight loss. e.g., 10 lbs in the last month.
○ Reasons for a diminished nutritional intake.
○ Anthropometric values: Body Mass Index (BMI) of less than 20 kg/m2 and calf circumference of less than 31 cm. You can use this user family BMI calculator from National Heart, Lung, and Blood Institute(Calculate Your BMI – Standard BMI Calculator (nih.gov).
○ Evaluate if you have problems with swallowing.
○ General muscular atrophy, loss of subcutaneous fat, muscle wasting.
Malnutrition treatment is a step-by-step process. Your doctor will ask why you have a poor intake or what is the reason behind losing muscles despite good intake. The treatment involves:

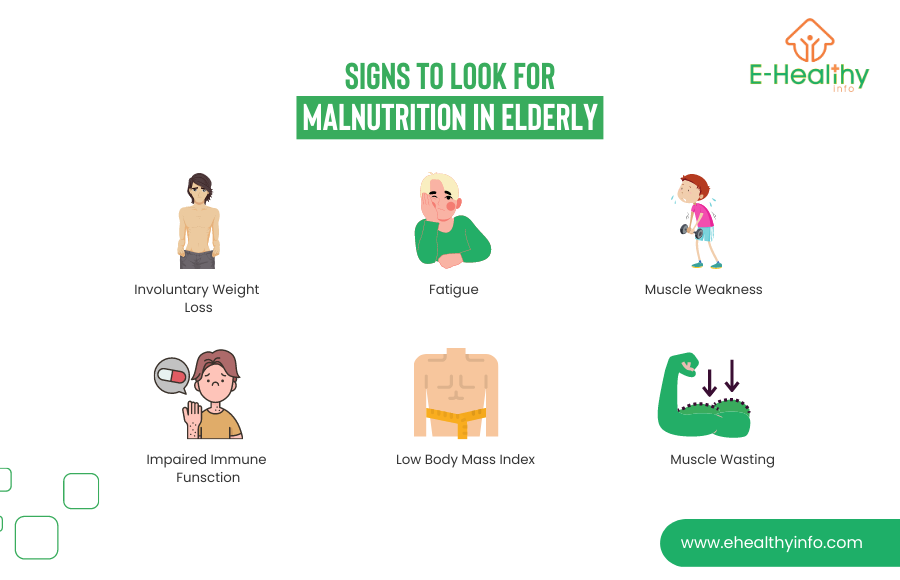
Involuntary weight loss
Fatigue
Decreased ability to fight off infections.
Low body mass index
Muscle wasting
Elderly people with poor nutrition are at a higher risk for malnutrition and physical health problems, which can further contribute to their decline in mental health. Adequate nutrition is essential for brain health systems and function and a diet lacking in essential nutrients such as vitamins B12, folate, and omega-3 fatty acids can contribute to depression, anxiety, and other symptoms including mental health problems. Some strategies that can help prevent malnourishment in this population include:
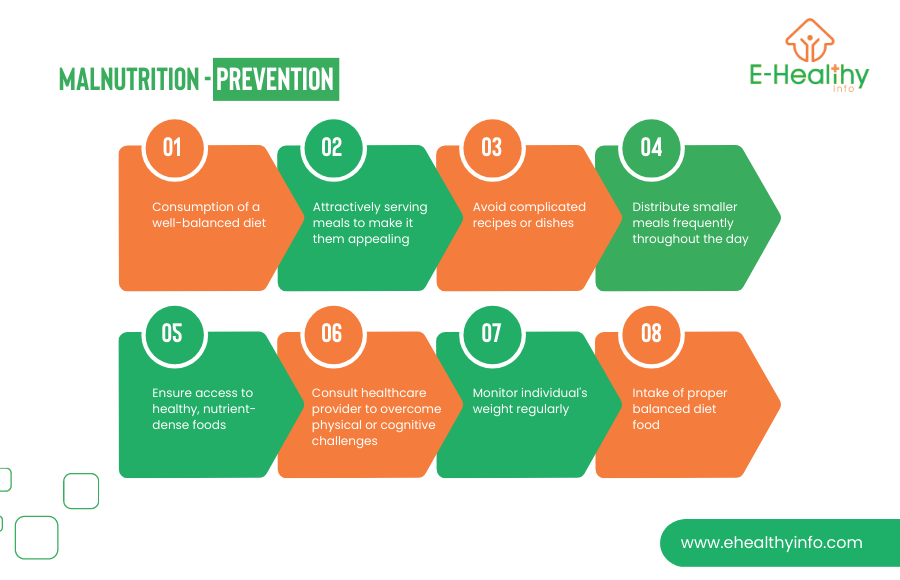
Make meals more appealing: Make meals more appealing by attractively serving them, using colorful plates and garnishes. Offer a variety of fresh food to make mealtime more enjoyable.
Keep meals simple: Avoid overly complicated recipes or dishes that may be difficult to chew or swallow.
Make sure the individual has access to healthy fresh food: Ensure that the individual has easy access to healthy, nutrient-dense foods, and consider delivering meals if necessary.
Address any physical or cognitive challenges: If the individual has physical or cognitive challenges that make eating difficult, work with a healthcare professional or occupational therapist to find ways to overcome these challenges.
Monitor the individual’s weight: Regularly monitoring the individual’s weight can help to identify any potential malnourishment early on so that it can be addressed promptly.
All older adults need the same type of diet.
Older adults should avoid all dairy products.
Supplements can replace a healthy diet.
Add dried fruit, chopped nuts, bacon pieces, cheese, mayonnaise, and avocado as a topping, and use butter or olive oil when cooking which will increase calorie intake without increasing volume.
Spread meals into several small ones throughout the day rather than just three large ones.
Higher-calorie beverages such as whole milk, shakes, smoothies, and oral nutritional supplements can be taken between meals instead of alongside meals.

Hickson, M. (2006). Malnutrition and aging. The postgraduate medical journal, 82(963), 2-8.
Norman, K., Haß, U., & Pirlich, M. (2021). Malnutrition in older adults—recent advances and remaining challenges. Nutrients, 13(8), 2764.
Ervin RB. Healthy Eating Index scores among adults, 60 years of age and over, by sociodemographic and health characteristics: United States, 1999–2002. Advance data from vital and health statistics; no 395. Hyattsville, MD: National Center for Health Statistics. 2008
Malnutrition in Older Adults: What to Watch for and How to Help. (n.d.). ASA Generations. https://generations.asaging.org/malnutrition-elders-how-help
Bauer, J. M., Volkert, D., Wirth, R., Vellas, B., Thomas, D., Kondrup, J., … & Sieber, C. C. (2006). Diagnosing malnutrition in the elderly. Deutsche Medizinische Wochenschrift (1946), 131(5), 223-227.