Atrial Fibrillation -Effective Treatment Strategies for AFib

What is Atrial Fibrillation (Afib)?
Atrial fibrillation, also known as AFib, is the most common type of treated arrhythmia, arising from an issue with the heart’s electrical system. In AFib, electrical signals originate from a location other than the sinoatrial (SA) node. These signals are rapid and compete for the conduction pathway, leading to a state of chaos. Subsequently, the normal coordination of the electrical signal that traverses the heart becomes disrupted; instead of a synchronized progression, the electrical impulses become disorganized. This causes the heartbeat to become quick, irregular, and less efficient. Compared to a healthy heart’s rate of 60-100 beats per minute, the atria start contracting over 300 times per minute. Consequently, blood is not effectively pumped through the heart during episodes of atrial fibrillation.
What Are the Symptoms of Atrial Fibrillation or Afib?
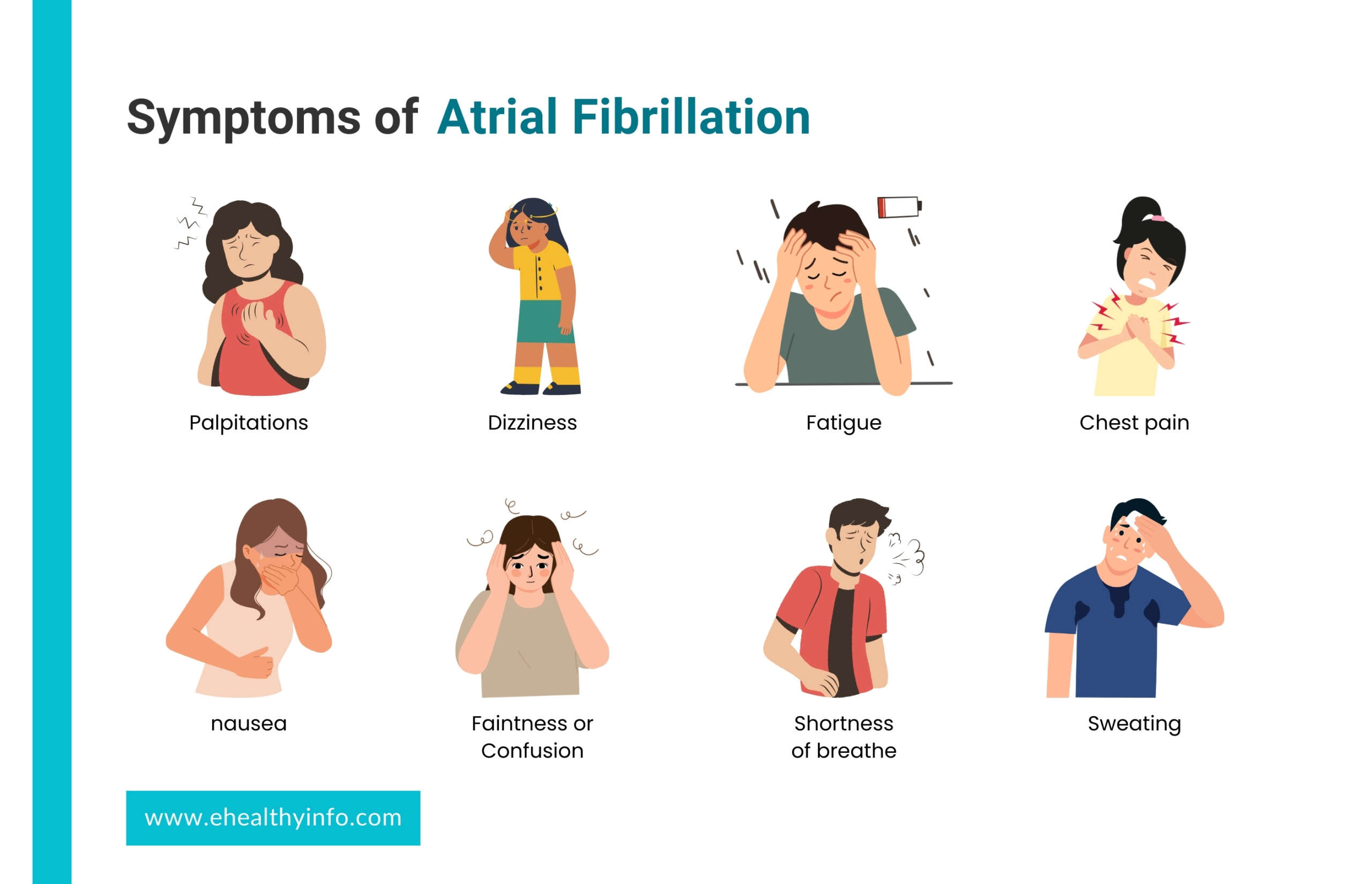
Many people with atrial fibrillation do not have any symptoms and may not be aware of them. However, you may experience palpitations (fluttering sensation in your chest), shortness of breath, chest pain, dizziness, nausea, fatigue, faintness or confusion, and sweating. You may also have trouble with everyday exercises or activities and experience pain, pressure, tightness, or discomfort over the chest.
What Are The Risk factors of Atrial Fibrillation?

Atrial fibrillation is frequently caused by heart disease. These include heart failure, heart valve disease, hypertension, and heart attacks(5 warning signs of heart attack). Obesity, sleep apnea, chronic obstructive pulmonary disease, abnormal heart structure, hyperthyroidism, and alcohol intoxication are other risk factors associated with atrial fibrillation.
Why is There a Risk of Stroke in Atrial Fibrillation?
The rapid, chaotic heartbeat means less time for the atria to relax and contract, resulting in slowed blood flow. When blood does not flow smoothly, there is an increased chance of clot formation in the heart. The blood then can carry these clots to other body areas, called as thromboembolism. These moving clots can be dangerous as these clots get wedged when reaching the smaller blood vessels and decrease blood supply downstream. A blood clot lodged in small blood vessels in the brain reduces blood flow to the brain and causes injury to the brain leading to ischemic stroke. Without treatment, AFib can also cause the ventricles to beat too fast. Over time, this weakens the heart muscle and leads to heart failure.
Your stroke risk depends on age and other risk factors such as heart disease, high blood pressure (hypertension), diabetes, or vascular disease. The CHA2 DS2 -VASc stroke risk tool helps doctors quickly measure your risk of stroke. Each major stroke risk factor carries points. By adding these points, your doctor can determine your stroke risk. Higher total points mean a higher risk of stroke. Your doctor will ask questions about heart and vascular problems and other risk factors for stroke and calculate the risk to see if you need a blood thinner to prevent a stroke.
How is a Diagnosis of Atrial Fibrillation Made?
Your doctor can detect atrial fibrillation in many ways:

- Using a stethoscope to listen to the heart
- Checking your pulse
- Electrocardiogram (ECG)- a test that detects electrical activity in the heart using sensors on the skin over the chest,
- Wearing a Holter monitor, a portable ECG with sensors on the chest, worn around the waist for 24 hours to several days,
- Several other mobile cardiac monitors, like Holter, are worn for extended periods. It monitors the heartbeat when it is normal and will trigger a recording when it senses an abnormal rhythm.
- An intermittent event monitor is always carried by the patient and placed on the chest when the symptoms occur. The rhythm recorded during symptoms is transmitted over the phone for review.
- Echocardiogram: Ultrasound of the heart to view heart function and heart valves and see if there are any clots.
How is Atrial Fibrillation Treated?
Your doctor individualizes the treatment strategy, considering your medical history and symptoms. Let’s look at some of the possible strategies:

- Rate control: Your doctor may prescribe drugs that lower heart rate and alleviate symptoms and stabilize heart function, such as β-blockers (e.g., metoprolol or carvedilol) and calcium channel blockers (e.g., diltiazem) or digoxin. If medications are not working, you might benefit from ablation of the conduction system, or if your heart rate goes too low while on drugs, you might need a pacemaker.
- Rhythm control: Rhythm control approaches include antiarrhythmic medications, electrical cardioversion, and catheter ablation. These interventions aim to reset the heart’s rhythm and prevent AFib episodes. Rhythm control may be preferred in certain situations, such as when AFib symptoms are severe, recurrent, or significantly impacting the patient’s quality of life. Your doctor may cardiovert your hearts rhythm to a regular sinus rhythm. Electrical cardioversion is a procedure that involves delivering a shock to the heart to restore normal electrical activity. If AFib returns and causes symptoms, your doctor may prescribe antiarrhythmic drugs for long-term use. Antiarrhythmic drugs help maintain a normal rhythm.
What Are the Surgical Procedures for Atrial Fibrillation?
1. Catheter Ablation
Catheter ablation involves inserting catheters into the heart to eliminate AFib sources and reduce the number of AFib episodes. Medications can control and maintain a regular heart rate by slowing the electrical signal traveling through the AV node. For patients who don’t have an optimal response to medications, ablation (a procedure that uses heat or cold energy to create tiny scars in the heart to block faulty electrical signals and restore a typical heartbeat) might be the better option.
This procedure destroys the tissue responsible for the arrhythmia. Ablation is not always successful and can result in serious complications such as infection, bleeding, or stroke in rare cases. The risk of recurrent atrial fibrillation is most significant in the first few weeks following the procedure. Sometimes, a pacemaker may be implanted in the system to ensure that your heart generally beats adequately after removing the problematic tissue. If this occurs, your provider may decide to repeat the process.
2. Plugging or Closing Off The Left Atrial Appendage(Watchman Device)
The left atrial appendage is a small sac in the muscle wall of your left atrium, known as the left atrial appendage. If you cannot take blood thinners, this procedure prevents clots from forming in the area and causing a stroke. This procedure may be performed concurrently with surgical ablation or cardiac surgery by your provider.
3. Watchman Procedure For Afib
By closing off the left atrial appendage, blood clots that form within the left atrial appendages are prevented from entering the bloodstream. The device has been shown in clinical trials to provide comparable effectiveness in stroke prevention to warfarin.
What Are the Measures to Prevent Atrial Fibrillation?

- Manage high blood pressure.
- Avoid excessive amounts of alcohol and caffeine- Overusing alcohol and stimulants can lead to abnormal heart rhythms, such as AFib and stroke.
- Eat a heart-healthy diet low in salt, saturated fats, trans fats, and cholesterol.
- Don’t smoke
- Control blood cholesterol
- Maintain a healthy weight
- Manage sleep apnea- If you have sleep apnea, your doctor may prescribe a mask or a treatment called a continuous positive airway pressure (CPAP) machine to ensure you get average amounts of oxygen while you sleep.
What is an Arrhythmia?
The heart normally beats 60 to 100 times per minute, with the beats occurring at regular intervals, creating a steady rhythm. However, when there is any disruption or abnormality in the usual sequence, rate, or coordination of the electrical impulses that regulate the contraction and relaxation of the heart chambers, the beats become irregularly spaced. This irregularity in the heartbeat is known as an abnormal heart rhythm or an arrhythmia.
What Are a Pulse, Heart Rate, and Heart Rhythm?
The blood circulation that occurs with each contraction of the heart is what we feel as the pulse in our body. The number of times the contraction of the heart occurs in a minute is what we call heart rate. When the SA node generates regular electrical impulses, the heart’s chamber contracts consistently and in a steady pattern, referred to as a regular heart rhythm. In simple terms, the regularity of your heartbeat is commonly called heart rhythm.
How Does the Electrical System in a Healthy Heart Work?
The heart consists of four chambers, i.e., two atria and two ventricles. Electric signal regularly originates in a small bundle of tissue known as the sinoatrial (SA) node, located in the right atrium- the upper chamber of the heart. It travels along a particular route in the heart called the conduction pathway.
Following the generation of the signal at the SA node, the atria contract, causing blood to flow from the atria into the ventricles. The signal is then routed through the atrioventricular (AV) node and into the muscle surrounding the ventricles leading to the contraction of the ventricles. When the ventricles contract, blood is pumped to the lungs and the rest of the body. This completes one cycle of heart contraction, and the next occurs with the generation of electrical impulses from the SA node.
Questions For Your Doctor
- If you have been diagnosed with AFib or suspect that you may have the condition, here are some questions that you may want to ask your physician:
- What is the cause of my AFib?
- How can I be sure I have AFib, not another severe heart rhythm problem?
- Will my condition go away on its own?
- What risks will it become worse (impact my life more)?
- Am I at increased risk of having a stroke?
- What are my treatment options?
- What are the risks and side effects of medications to control my condition or reduce the stroke risk?
- What are the risks and benefits of other treatment options?
- Should I see an electrophysiologist (a specialist in heart rhythm disorders)
References
- https://www.heart.org/en/health-topics/atrial-fibrillation/why-atrial-fibrillation-af-or-afib-matters
- https://www.heart.org/en/health-topics/atrial-fibrillation/treatment-and-prevention-of-atrial-fibrillation/surgical-procedures-for-atrial-fibrillation-afib-or-af
- https://www.heart.org/en/health-topics/atrial-fibrillation/treatment-and-prevention-of-atrial-fibrillation/prevention-strategies-for-atrial-fibrillation-afib-or-af
Return to Home
